On Tuesday, October 23, Ensign was invited to participate in the closing bell ceremony for NASDAQ. This is a great honor and comes almost to the day of our 5 year anniversary of becoming a public company. If you missed it, you can visit the NASDAQ MarketSite to read the article: The Ensign Group, Inc. Rings The NASDAQ Stock Market Closing Bell and view the entire ceremony. When you bring up the video clip it may seem to do nothing for a while because what you are seeing are photos of our team being displayed on a huge billboard in Times Square. If you click on and hold down the two fast forward arrows it will bring up the presentation faster.
Team Building at Park Manor
 Ever feel at a loss for words when wanting to express your appreciation for your awesome therapy team? Sonya Taylor at Park Manor Rehabilitation Center in Walla Walla, WA, found a way to allow for her therapists to express their gratitude and appreciation for one another using a team building exercise that turned 360 degree feedback into 360 degree love for one another. Each therapy staff member wrote down one thing they appreciated or admired about each team member. Sonya then gathered the notes and wrote them on individualized “You Rock” cards for every team member. What a great way to highlight and celebrate the unique strengths of your therapists!
Ever feel at a loss for words when wanting to express your appreciation for your awesome therapy team? Sonya Taylor at Park Manor Rehabilitation Center in Walla Walla, WA, found a way to allow for her therapists to express their gratitude and appreciation for one another using a team building exercise that turned 360 degree feedback into 360 degree love for one another. Each therapy staff member wrote down one thing they appreciated or admired about each team member. Sonya then gathered the notes and wrote them on individualized “You Rock” cards for every team member. What a great way to highlight and celebrate the unique strengths of your therapists!
PRN Appreciation
 PRN Appreciation Program happening now at select facilities!
PRN Appreciation Program happening now at select facilities!
Cloverdale, CA
Ukiah, CA
Willits, CA
Youngtown, AZ
Reno, NV
For each 4 hour shift worked, therapists will get a chance to win an iPad which will be given away in November. The more shifts worked, the more chances to win!
Refer for more points! A referral of a PRN, part time or full time therapist is worth an extra 10 points. (Each point is worth one entry form in the iPad giveaway!) If a PRN therapist chooses to be considered for a full time position at any of these facilities, they will also earn an extra 10 points. This program is running now through the last week of November with the iPad drawing taking place that week.
Watch for more fun therapy appreciation activities at a facility near you!
Kinesio Taping Seminar

Date: Nov 17 and 18, 2012
Time: 8 AM – 5:30 PM each day
(1 hour lunch break)
:
University of North Texas
Allied Health Center
Fort Worth, TX
Ensign Facility Services hosts seminars in facilities that are ADA accessible. Please let Jon Anderson, jonanderson@ensigngroup.net know if you need any special accommodation.
Instructor:
‘Dee’ Virginia Ellis, PTA, CKTI
Dee is a Physical Therapist Assistant who has practiced in many different settings and states. Dee specializes in aquatic therapy, Pilates based spinal stabilization and orthopedic outpatient rehab. She has been a PTA for 15 years, graduating with her A.A.S. from Community Colleges of Southern Nevada in Las Vegas with a Gerontology Wellness Specialty. She also did undergraduate study at San Diego State University in California. Dee has a special interest in wellness and prevention.
Dee has been a Certified Kinesio® Taping Practitioner for 8 years and has been a Certified Kinesio® Taping Instructor since 2005. Dee has her American Physical Therapy Association (APTA) Advanced Proficiency in the musculoskeletal realm and was the recipient of the Texas Physical Therapy Association’s (TPTA) Joy Davenport award in 2008. She is an active volunteer in the APTA, the TPTA and the Aquatic Section of the APTA. Dee has presented continuing education on Electrical Modalities, Aquatic Physical Therapy and Kinesio® Taping: Fundamentals and Whole Body Techniques.
Dee currently works for as a PRN for local south Texas hospital systems and home health agencies.
Topic:
Kinesio Tape Course (KT1 and KT2)
KT1: Fundamental Concepts & Basic Muscle Applications (To be taken in conjunction with KTAI approved KT2 course)
The KT1 course is designed to introduce practitioners to the Kinesio Taping® Method. During this eight-hour class, the instructor will introduce Kinesio Taping® concepts, theory and history, and discuss the four major physiological effects; skin, muscle, circulatory/lymphatic, and joint. During lab sessions, attendees will have ample time to practice Assessment Tests approved for the enhancement of their Kinesio Taping® skills and muscle applications for both the upper and lower body. Upon completion of this course, attendees will be able to discuss and apply the Kinesio Taping® Method to relax overuse syndromes, stimulate weak muscles, and decrease pain and swelling.
KT2: Advanced Concepts & Corrective Techniques (To be taken in conjunction with KTAI approved KT1 course – prerequisite is completion of KT1 course)
The KT2 course builds on material learned in KT1. During this eight-hour class, the instructor will introduce the six Corrective Techniques (Mechanical, Functional, Space, Fascia, Ligament/Tendon, and Lymphatic) and discuss their application in a variety of clinical conditions. During lab sessions, attendees will have ample time to practice applying these techniques to a variety of upper and lower body conditions. Upon completion of this course, attendees will be able to discuss and apply the Kinesio Taping® Method to orthopedic and neurological conditions.
COURSE OBJECTIVES
Upon completion of this course, the participant will be able to:
- Describe the concepts of Kinesio Taping.
- Review muscular anatomy as it is related to Kinesio Taping.
- Explain and apply the concepts of the Kinesio Taping Method.
- Describe the unique qualities of the Kinesio Tex Tape.
- Recognize the principles of Kinesio Tex Tape application.
- Utilize and demonstrate application skills in guided laboratory sessions.
- Demonstrate application skills during lab sessions.
- Practice the various cutting techniques and their clinical application.
- Apply Kinesio Taping method to relax and stimulate muscles.
- Apply Kinesio Taping methods for pain, swelling, joint mobility and stability.
- Apply various taping techniques for treatment of the spine, and upper/ lower extremity dysfunction
- Apply various taping techniques for treatment of unique conditions using the concepts and principals of the Kinesio Taping Method.
Who Should Attend? PTs, OTs, ATs, DCs, LACs, MTs, PTAs, OTAs and other medical practitioners. THIS COURSE IS INTENDED FOR LICENSED HEALTH CARE PRACTITIONERS ONLY
CEUS:
You can submit 16 hours continuing education credits to TX Physical Therapy Association. The Kinesio Taping Association is an approved provider for AOTA (Provider # 4489). The assignment of AOTA CEU’s does not imply endorsement of specific course content, products, or clinical procedures by AOTA. The Kinesio Taping Association is recognized by the Board of Certification, Inc. (BOC) to offer continuing education for certified athletic trainers (provider # P2293). Kinesio Taping Association is approved by the National Certification Board for Therapeutic Massage and Bodywork (NCBTMB) as a Continuing Education Approved Provider (Provider #450030-06).
Cancellation/Refunds:
No refunds
Class Schedule:
KINESIO TAPING® AGENDA
Day 1 – Fundamental Kinesio Taping
| 7:30 | Sign in |
| 8:00 | Instructor Introduction and Bio |
| 8:10 – 10:00 | Introduction to Kinesio Taping Concepts, Theory and History, Qualities of Kinesio Tape, Differences, Benefits and Finger Demonstration, introduction of Five Major Physiological Effects and Skin Function, Circulatory Function, KT Skin & Fascia Function, Iliocostalis Lumborum Demo Lab, KT Muscle Function and Basic App Concepts |
| 10:00 | Break |
| 10:15-11:30 | Joint Function; Biotensegrity; Application Basics, Directional Lab – Upper Trapezius, Challenges, Contraindications & Precautions, Intro to KT Assessment Tests |
| 11:50 | Q&A |
| 12:00 | Lunch |
| 1:00-3:00 | KT Cervical Flexion Assessmet, Longissimus Cervicis (Cervical Paraspinals) Application Lab, KT Cervical Extension Assessment, Scalenus Anterior Lab, KT Trunk Flexion Assessment, Rectus Abdominis App Lab, KT Pectoral Girdle Assessment, Pectoralis Major and Rhomboid Major Lab, |
| 3:00 | Break |
| 3:15 – 4:30 | KT Hip Rotation Assessment with Lab, Gluteus Medius App Lab, KT Leg Raise Assessment with Lab, Quadriceps Femoris App Lab, Review Five Major Physiological Systems, App Concepts, Assessment Questions, Extensor Digitorum Lab, Hamstrings Lab |
| 4:30-5:30 | Assessment Q&A; KT1 Review & Q&A, Application Requests; Conclusion |
Day 2- Advanced Kinesio Taping
| 8:00 – 10:05 | Overnight Responses, Troubleshooting, Assessment Questions, & KT1 Review, Basic Concepts of Corrective Techniques, Tension guidelines, & Precautions., Mechanical Correction, Y Technique with tension in the Tails and base, Mechanical Correction, I Technique, Mechanical Correction Lab: Patellar Tracking, Mechanical Correction, Shoulder Instability, Mechanical Correction Lab: Shoulder Instability |
| 10:05 | Break |
| 10:20 – 11:30 | Introduction to Fascia Correction, Fascial Oscillation and Gliding. “Y” Tension in Tails, Tension in Base, Rams Head., Fascia Correction, Y Technique with tension on the tails. Manual Fascial Glide Correction With Tension through the tails., Fascia Correction Lab, Fascia Correction, Y Technique with tension through the base. Manual Fascia Winding Correction Technique with tension in base., Fascia Correction Lab, “Y” Strip: Tension on Tails, Rams Head App, Fascia Correction Lab |
| 11:30 | Lunch |
| 12:30 – 3:10 | Introduction To Space Correciton. Space Correction “I” Technique, Space Correction “Donut Hole” App. Space Correction Lab, Space Correction “Star” App. Space Correction “Button Hole & I Strip” App. Space Correction Lab, Space Correction “Web” App and Lab, Introduction To Ligament/Tendon Correction, Ligament Correction, Tendon Correction “I” & “Y” Techniques, Ligament & Tendon Correction Lab |
| 3:10 | Break |
| 3:25 – 5:15 | Tendon Correcton with Plantar Fasciitis App, Tendon Correction With Plantar Fasciitis Lab, Introduction to Functional Correction, Function Correcton Technique, Functional Correction Lab, Introduction To Circulatory / Lymphatic Correction, Circulatory / Lymphatic Correction “Fan” Technique Lab, KT Clinical App Finger, Documentation, Billing, Precautions, Contraindications and Rules, Assessment Questions, Glossary Review, Application Requests and Q&A |
| 5:10 – 5:30 | Assessment Questions, Glossary Review, Application Requests; Q&A; Conclusion |
$569 for licensed professionals
$369 for students (limited space available)
Questions/Information/Sign Up:
Kelly Wallerstedt, Ensign Therapy Resource Assistant
Pay via paypal on ensigntherapy.com
Transforming Care at Brookfield
- The therapists didn’t let their inner-city location limit implementing a gardening program. They made use of a small space near the parking lot to help residents plant strawberries, tomatoes, jalapenos and bell peppers in different level gardening boxes.
- They found out there were some artistic abilities among the residents and the team developed an art class.
- The Brookfield Medical Director, Dr. Nguyen, helped to lead a kick-boxing class for facility staff to keep everyone healthy and active.
- The therapy team partnered with activities to start a computer literacy class for residents.
- The therapists got together and completed a “graduation kit” comprised of a safety education booklet, Physiotools exercises, a therapy group picture, and a graduation cap signed by the therapists with personal messages about their progress.
- The team partnered with Activities to start a pet-therapy program.
- The Therapy Team partnered with Activities once again to bring Tai Chi Qigong to the residents. A chiropractor student (Lito’s bother!) taught the class, and the residents learned how to integrate breathing, physical activity, and mental/spiritual health.
The Brookfield Therapy Program continues to inspire all of us. The ideas are simple. What is not simple is the magic that happens when this group of professionals comes together to love one another, to love their coworkers, and to love their patients so they can make a difference in lives day after day.

Gardening
The therapists didn’t let their inner-city location limit implementing a gardening program. They made use of a small space near the parking lot to help residents plant strawberries, tomatoes, jalapenos and bell peppers in different level gardening boxes.
Top 5 Steps to Developing a Managed Care Program
 Get patients to the next Level of Care in a shortened amount of time, with quality outcomes.
Get patients to the next Level of Care in a shortened amount of time, with quality outcomes.
The expectation is that patients will achieve their highest level of function with the support of community resources (eg., Home Care, Outpatient therapy.)
 Manage clinical needs and financial implications according to contracted levels.
Manage clinical needs and financial implications according to contracted levels.
Pay attention to over and under utilization of therapy.
Negotiate a higher level of care/reimbursement rate if patients can tolerate more therapy.
 Goals should be written according to specific prior level of function.
Goals should be written according to specific prior level of function.
 Begin working with patient/ family from day 1 to determine a reasonable and achievable discharge plan.
Begin working with patient/ family from day 1 to determine a reasonable and achievable discharge plan.
Drive the d/c date from the time of admission.
Be mindful of the health plan goal = decreased LOS/ next Level of care.
 Meet weekly with the clinical team to discuss progress/ barriers to goals.
Meet weekly with the clinical team to discuss progress/ barriers to goals.
Discuss the PLOF with the entire team after admission; they may have valuable information to add from discussions with the family.
Address the D/C plan every week to ensure it is reasonable. If not, evaluate alternative options with the patient/ family quickly.
Work with your Administrator to ensure you have assigned one, knowledgeable person to effectively communicate skilled therapy services provided, goals/ barriers, estimated LOS, and the discharge date/ plan weekly with the health plan case manager.
Integrating Care: Challenging Behaviors
Understanding, Preventing and Managing Challenging Behaviors – A Cognitive Link
By Pat Jakubiec, Clinical Resource
Challenging behaviors are one of the most stressful aspects of care giving. They result in caregiver stress, excess disability and increased care costs. Recent research suggests that pharmologic approaches are not always effective and they can cause potentially harmful secondary side effects, including an increased risk for falls. Research shows promise for engagement in meaningful activity tailored to an individual’s ability can reduce depressive and agitated behaviors as well as reduce caregiver stress.
Behavior is a way individuals express a need or desire. It can result from an emotion, and sometimes the behavior remains the focus not the emotion (Pollard, 2005). Individuals with cognitive disabilities can be misunderstood and sometimes blamed for their behavior. The reason is usually related to underlying neuro-biological causes that include global cognitive abilities, speed of brain function and personality traits.
Every change in a person’s environment will require the individual to cope and adapt, using extra effort and energy. Many people with cognitive impairment are not able to learn to adapt to new routines, procedures and physical changes in the environment. The individual biologically has difficulty noticing and processing information, therefore they cannot use the information to influence behavior. Functional performance beyond an individual’s ability cannot be expected especially in novel situations. When this occurs, performance failures can be anticipated.
Some researchers describe the anterior cingulate cortex of the brain as a key area between thought emotion and the body’s response to what the brain is feeling. An individual’s responses represent value judgments within a social context. The individual with cognitive disability often times has difficulty understanding the full scope of the social environment and difficult behaviors can represent this challenge. When the brain declines in its ability to work as a global unit, agitation can be viewed as a loss of control over behavior and the ability to process the environment.
There is a fine balance between doing too much for the individual that may lead to depression, excess disability and a decreased sense of self. Doing too little can result in agitation, problematic behavior and an increased risk for accidents. It is important to assess an individual’s abilities and personal factors in the context of holistic assessment. The degree or level of behavioral reaction can be attributed to an individual’s personality traits and how they have handled life situations.
In 1995 Cohen-Mansfield described behavioral symptoms into 4 groupings:
- Physical aggressive behaviors
- Verbally aggressive behaviors
- Non-aggressive physical behaviors
- Non-aggressive verbal behavior
A careful medical assessment needs to be included. Certain conditions and illnesses, unmanaged pain, and medication changes all need to be considered.
Environmental assessment and management become critical. Changes in the physical environment can cause challenges as the person may have difficulty processing the physical space. Consistent nurse aide assignments with ongoing team education provide a supportive human environment. Integrating lifelong habits and routines promotes cognitive strengths and a sense of self. An integrated environment promotes overall feelings of well-being and security.
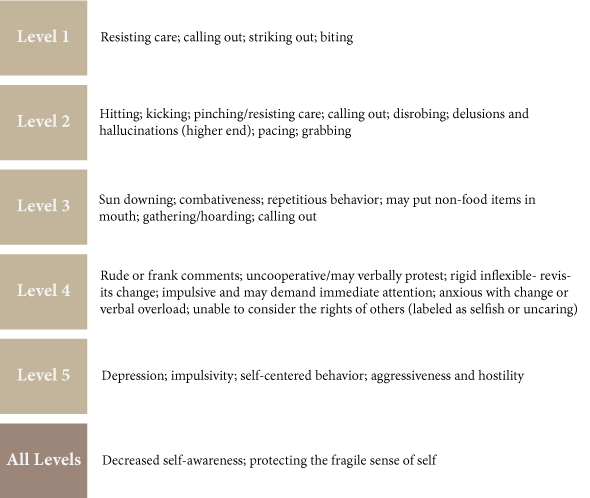
Use of the cognitive disabilities model allows healthcare clinicians to understand different levels of global brain activity. The six levels (ACL scale) describe distinct patterns of behavior that can be anticipated. These behaviors can be measured and managed by skilled clinicians, offering a cognitive systematic approach to management and intervention. Strategies can be developed integrating personal factors that can be employed by everyone. This provides a pro-active approach to care and may prevent some challenging behaviors before they occur.
Behavior Patterns Observed in the ACL Scale
Bathing Challenges/Process
Resisting care, especially during bathing is a common challenge that causes distress for both the individual and the caregiver. Interventions are meant to be used as a guideline and are meant to be modified by the treating therapist in the context of a comprehensive holistic assessment.
Reasons for referral
- Recent decline in function and or participation
- Resisting care- verbal or physical aggression
- Refusing or withdrawal
- Individuals requiring more than one nurse aide to complete bathing /showering
- Issues of safety associated with bathing and showering
Evaluation
- Complete a comprehensive holistic assessment
- Establish a functional cognitive level through the use of at least 2 standardized tools and observe a stable pattern of behavior
- Have the family complete an Advance Lifestyle Directive “Life Story gathering instrument.” Gather as much data related to the person’s lifelong bathing/ showering habits to include time of day, types of products used, frequency, preferences etc.
- Observe the person and caregiver in the actual task environment
- Identify problem behaviors observed and any identifiable patterns of difficult behaviors. (frequency, duration intensity)
Intervention
Clinical analysis of behaviors. Many behaviors can be an expression of an unmet need. This may include:
- Feeling cold; fear; pain
- Embarrassment/vulnerability
- Loss of control
- Not able to process the environment, or understand what is happening
- Fatigue
- Unable to understand what the caregiver is communicating
Compare cognitive level with actual task participation. If excess disability is present determine why and what therapy interventions can be done to improve participation. When excess disability is cognitively related sometimes the caregiver approach can be modified to improve outcomes. This is often witnessed when people are functioning in Allen Cognitive Level (ACL) 3.
Develop a plan to reduce problematic behaviors, maximize patient participation and profile effective communication. Things to include in the plan are:
- Time of day (avoid bathing when fatigue is present, life habit)
- Use of familiar items
- Integration of preferences and lifelong habits/ mode of bathing
- Communication strategies
- Physical environment considerations (room temperature, water temperature, unfamiliar location or change, privacy, noise level, past familiar environment, comfort)
- Pain management strategies
- Strategies for participation
- Safety
Provide treatment sessions to implement and modify strategies and to train the caregiver in the actual task environment.
Document the plan and caregiver training.
Develop a functional maintenance program.
Follow-up with caregivers during and after the procedures have been completed, and note what has been successfully achieved.
Conclusion
This information was adapted from the VCIM Clinical Guide for Understanding, Managing and Preventing Challenging Behaviors. Some of the facilities using this approach have shown a reduction in falls, combative behaviors, reduced use of restraints and reduced use of psychotropic medications. For more information, contact Pat Jakubiec at pjakubiec@ensigngroup.net. Onsite clinical development and training sessions and skype case study consultation are available. Staff development and training is tailored to individual program needs.
Reaching Out to the Community
Val Montoya is a PTA at Southland Care Center in Norwalk, Ca, with a B.S. in Exercise Physiology, and a dream to teach and train mobility and wellness in the elderly population. When Southland’s CEO, Jim Morrison, met with a nearby Assisted Living Facility to see how we could be a part of health and wellness in their facility, it was a perfect way for Val to pursue her dreams while educating and helping within the Norwalk community.
 Val teaches an exercise class at Vintage Cerritos every Wednesday morning; the class changes monthly based on the needs and desires of the residents. Her first class started with a handful of curious folks, and within weeks they were up to over 30 residents and needed to expand the class to the library. Fall prevention and safety is a big part of her class, and the residents have given feedback that they feel more confident and stronger since taking Val’s class and implementing safety techniques back in their apartments.
Val teaches an exercise class at Vintage Cerritos every Wednesday morning; the class changes monthly based on the needs and desires of the residents. Her first class started with a handful of curious folks, and within weeks they were up to over 30 residents and needed to expand the class to the library. Fall prevention and safety is a big part of her class, and the residents have given feedback that they feel more confident and stronger since taking Val’s class and implementing safety techniques back in their apartments.
This partnership is a wonderful example of how being best FOR the community can help our staff members grow while developing partnerships with those in the continuum of care for our elderly.
If ALF employees are potential Medicare / Medicaid patient referral sources, then it is not appropriate to provide a class at no cost to the ALF as that would potentially violate the Anti-Kickback Statute. Best practice is to charge the ALF a fair market fee for the classes in order to protect yourself and the ALF. Remember, Anti-Kickback violations implicate both the giver and receiver of a kickback.
Where Does that Tube Connect?
Teamwork is the Key to Success in Sub Acute Care
By Elyse Matson, MA, CCC-SLP, Carmel Mountain Rehab & Healthcare Center, San Diego, CA
As we all gathered Monday morning for our weekly rounds to our patients, it occurred to me that we really are a TEAM. Although we hear that word so much in our work, this was starting to look more like the Webster’s definition: “cooperative or coordinated effort on the part of a group of persons acting together as a team or in the interests of a common cause.”
A few years back when we were first launching our Sub-Acute unit, there was some apprehension in rehab as we were unsure of our role on this new unit. How would our skills fit into this new set of patients? Even questions as simple as, “How do we move these patients?” were being asked. As training began and the unit took shape, it was clear that rehab could take its place on the team along with many other disciplines.
I remember when we received orders to see our first patient—he was on a tracheostomy tube and ventilator. The first time we placed a Passy-Muir Valve on this patient, and he spoke clearly to the staff and family, it was one of those a-ha moments. As the nursing and respiratory staff began to see how speech therapy might be utilized with these patients, we knew we could create something special. Less than a week later, physical and occupational therapy assisted that same patient out of bed and walked with him down the hall. Everyone saw we were not just going to sit idly by and care for bedbound patients. We were here to do what we always do—rehabilitate the patient to their highest potential, whatever that is.
Over the last two years of working with these incredible patients, we have worked together as a team to develop protocols, policies and procedures, and, in the process, helped many patients. We have even seen a few of our patients who were on ventilators return to visit by walking in the door unassisted.
When we review each patient with the team every week, we address issues involving their medical care, psychosocial needs, nutrition and, of course rehab. Our Director of the Sub Acute Unit and lead Pulmonologist facilitates our meeting.
Because he is there, we can make changes to the patient plan of care with ease. For example, if a patient is starting to eat, we can change the tube feeding schedule right then. If we want to evaluate a patient for tolerance of the Passy-Muir Valve, we can discuss the parameters and schedule a time to evaluate this with respiratory therapy and/or nursing. Everyone is then aware of the plan.

True Colors
One of the most popular personality tests is the True Colors Personality Test. This personality test has participants choose words that best describe themselves. The test will then rate one’s personality as either a blue, green, orange or gold personality type.
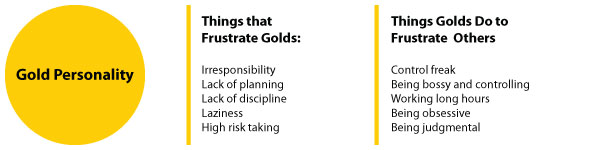
You may be a combination of two colors, but usually an individual will exhibit one primary color. By using a personality test, it allows leaders to understand the personality attributes associated with various team members.
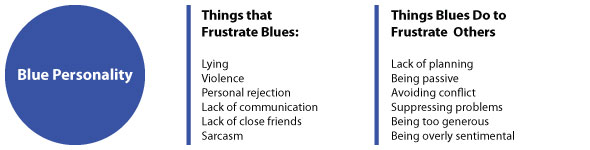
As managers and leaders, we may operate as one primary color for the most part, but high levels of stress and other environmental factors can shift one’s personality type for short intervals.

As a rule of thumb, you should recognize your strong attributes and keep in mind the attributes that irritate people.
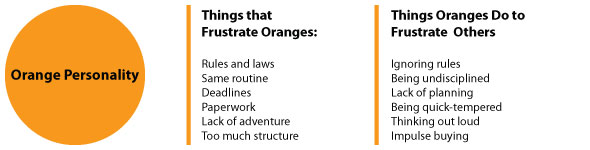
Introducing True Colors to the world over 30 years ago, True Colors International is the originator of using colors to represent the four personality styles, and remains the preeminent source for workshops and certifications in the True Colors methodology across the world.