Submitted by Stephanie Cole, Bandera Therapy Resource – Arizona
In the spirit of Passion for Learning I would like to share an INCREDIBLE Capstone project with all of you. I am hoping you can use some of the tools in your own buildings!
Kyle Higgins, DPT, our fearless DORITO and DPT extraordinaire at Montecito Post Acute Care & Rehabilitation in Mesa, AZ, is the creator. Kyle has been invaluable to our therapy program, demonstrated excellent clinical skills, leadership and dedication to hundreds of our most difficult patients. It is with great pleasure I share his story and all of his hard work. Please feel free to reach out to Kyle directly with any questions about the forms/tools.
In Kyle’s words:
For my project, I wanted to capture all of the fun insurance rules/guidelines that are pertinent to therapists and turn them into an easy chart. In the past year, we have had multiple new hires, with several of them being new grads. I love teaching and helping them in any way I can, but I often caught myself doubting what I was teaching due to insurance guidelines constantly changing and to be honest, just SO many rules. Thankfully, this chart has been helpful for me and even for our therapy vets as a refresher! I hope this project can be as helpful to other facilities and therapy resources as it has been for Montecito.
I have included a general Insurance Guidelines and LTC Insurance Guideline document that captures general rules for various payers that we have been successfully using at Montecito.
Additionally, during this DORITO program, I have created and implemented a PDPM checklist that our evaluators are using (and MDS director loves). I know the therapy portal had several PDPM checklists already. However, most of them did not seem to include consistent information, so I made one that encompassed everything from every checklist.
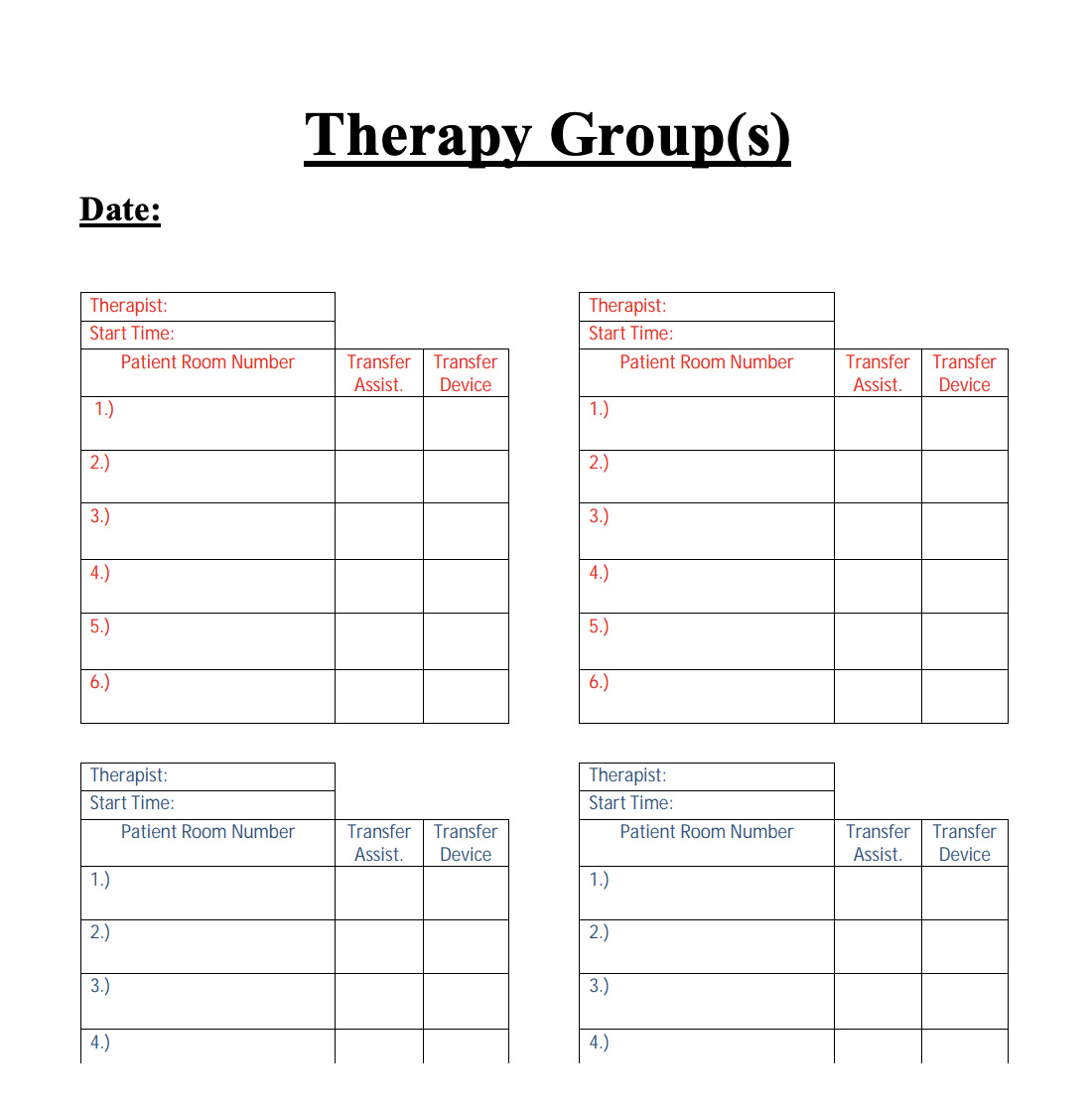
Lastly, I have created an IDT communication board. Stephanie Cole and I printed/laminated over 300 copies. We hung hooks on the cabinets in every room and hung the hole punched sheet with a ring for each patient. On eval, the evaluator will fill out the sheet with a dry erase marker. As patients progress, whatever therapist that is working with the patient can update the sheet. Hopefully, this will continue to improve the communication between nursing and therapy. But most importantly, hopefully this has improved the safety of our patients