By Sarah Scott, DOR, Draper Rehabilitation & Care, Draper, UT
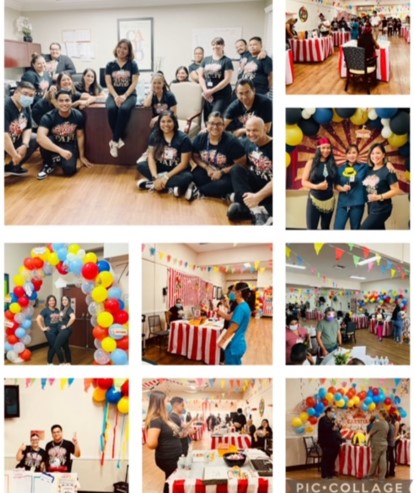
Draper Rehabilitation and Care Center is located one block from Historic Draper Park. Recreational, Physical, Occupational, and Speech therapy have coordinated to hold large group activities at the park every other Thursday through the good weather month. It is an “all hands on deck” effort to get the residents ready, sunscreen coated and over to the park. Why go through this effort? The answer is simple. The residents love it and it is the kind of activity almost everyone throughout their life has participated in and enjoyed. Who has not spent part of a Spring or Summer day enjoying the sunshine at a park?
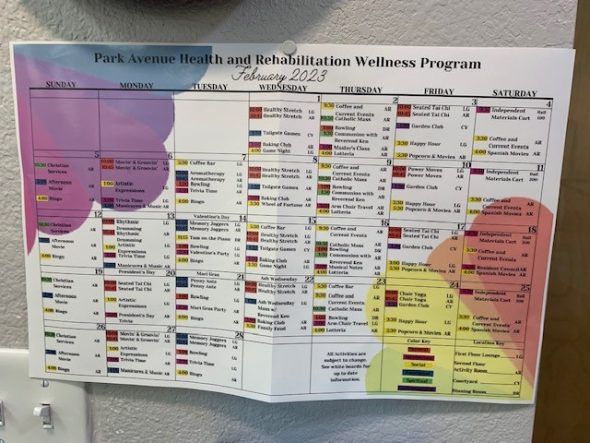
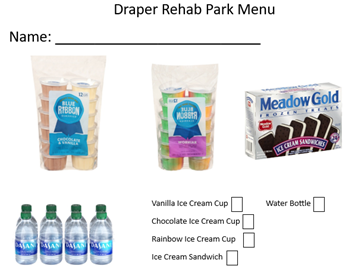
For this week’s activity at the park, PT/OT/ST all had prepared activities lasting 15 minutes each. The residents were grouped in three shady areas and the therapy teams travelled from group to group in 15 minute intervals so that all had the opportunity to perform each activity. Recreational therapy and selected CNA staff supported all of the residents preparation, attendance, participation at the group. Jeremy Meldrum, ED at Draper Rehab, dragged a cooler loaded with treats and took each resident’s “order” to support a community activity where each resident could select and order a treat using a prepared “menu”.
The Physical Therapy group worked out dynamic balance and upper body strength with a bowling game where residents rolled a ball across the lawn into a basket with different point values depending on the location and difficulty of the roll. Occupational Therapy challenged core strength, proprioception, and upper body function with heated rounds of cornhole. Speech Therapy targeted the essential skill of respiratory support for speech and swallow with bubble blowing and environmental awareness and reasoning skills to identify items around the park. Residents cheered each other’s success and chucked together at misses. Function, Fun, Freedom. We are collectively looking forward to the next group outing to the park!

The OT group enjoyed the fresh air and upper body workout as they launched beanbags for a round of cornhole.

Speech Therapy exercised everyone’s lungs with a bubble blowing activity and mind with identification of items around the park. Respiratory support is essential for speech intelligibility and swallow.
It was a beautiful day for the residents. As one resident stated, “It is so great to get out!” It is always a bit of organized chaos and we collectively learn from each activity. Can’t wait to see the smiles and laughter in two weeks!