By Justin Cruz, COTA, The Hills Post Acute Care, Santa Ana, CA
At The Hills Post Acute, we work with our residents across all disciplines to enhance
their quality of life and have them become the best person they can be. We meet a variety of
personalities that always manage to surprise us, keep us humble, and reaffirm our passion for
therapy. As a multidisciplinary team, we believe that mutuality, consistent feedback, and
collaboration between the residents and therapy team helps create the most effective therapeutic
interventions.
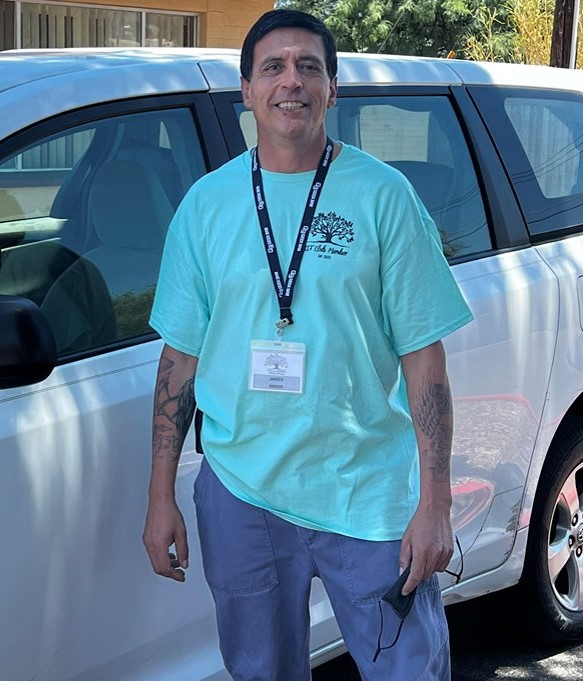
Today, we would like to put the spotlight on one of our long time residents who took our
well intentioned efforts to heart: Mr. R. When Mr. R came to The Hills Post Acute near the
beginning of 2020, he was a very different person. Mr. R experienced a great fall that rendered him very weak, apathetic, and socially withdrawn. However, we did not give up and we continued to bring him to therapy where we provided encouragement and motivation to him almost everyday.

As time passed, our relationship with Mr. R gradually grew and he began to participate in
every activity the therapy team provided him. Mr. R’s condition improved as his strength
increased and he became more sociable with the other residents. He listened to our feedback and
provided us with feedback of his own on what he wanted to focus on.
Currently, Mr. R continues to participate in therapy almost every day with such interest and enthusiasm that it brings a smile to our face and a sense of pride to what therapy can achieve. To us at The Hills Post Acute, Mr. R is our success story.