At Hurricane Health and Rehabilitation, we have seen time and again that collaboration improves patient outcomes. Take, for example, the case of Phil, a 50-year-old resident who arrived at our facility after sustaining a bilateral anterior cerebral artery infarction (ACA CVA). Phil sustained damage to both hemispheres of his frontal lobe with corpus callosum involvement.
Having been discharged from our local hospital’s acute rehab unit due to failure to comply with the required therapy regime, Phil came to Hurricane Health with unique requirements. With such a rare stroke, Phil needed a therapy team willing to collaborate not only amongst ourselves, but also with the healthcare community to create and execute a successful plan of care.
The Problem
Phil was alert and pleasant, but he also was described as apathetic and unwilling to cooperate by the neuro specialty rehab unit at the local hospital. His deficits included difficulty following simple commands, incontinence, minimal response when asked questions, occasional volitional speech, poor initiation of gross motor movements, and an inability to communicate with staff to express wants and needs.
Finding Solutions
Phil’s condition did not improve after two weeks of traditional therapy approaches. Preliminary research revealed that Phil’s behaviors were common sequelae of bilateral ACA CVA, rather than therapy avoidance behaviors. Therapists shared findings from treatment sessions to create a clear picture of Phil’s deficits and preserved skills. Together, we discovered he presented with symptoms characteristic of akinetic mutism.
The Opportunity
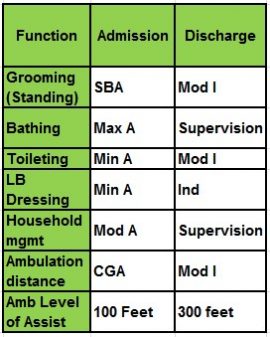
Now that Phil was communicating effectively with staff and family and initiating ADL routines, he was able to participate in more rigorous physical and occupational therapy. He began to make progress with gross motor movements as well.
Meanwhile, speech therapists collaborated with OT Asa Gardine to address bowel and bladder care. Using Phil’s own cell phone, we programmed alarms every three hours and trained him to request assistance to the restroom at these scheduled times. Input from both therapies was critical to implement such an effective bowel and bladder program.
Collaboration
Evidence-based therapy approaches for Phil’s akinetic mutism were not readily available. Phil’s speech therapists, Karen Straw and Maggie Maxfield, reached out to experts in this field of research to learn about effective techniques.
We were contacted by Danielle Erdman, a speech therapist with Brooks Rehabilitation in Jacksonville, Florida. She studies a phenomenon called the “telephone effect,” or the transient improvement of communication skills when patients with akinetic mutism speak over the telephone, rather than face-to-face.
Through our collaboration, we crafted a unique therapy plan that relied on the telephone effect to improve Phil’s communication skills. We saw rapid improvement in all of Phil’s communication deficits, with sufficient carryover away from the telephone — a novel finding that is being prepared for publication by Erdman, et al.
Outcomes
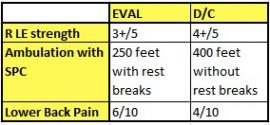
Undoubtedly, collaboration proved to be the key to identifying the best therapy approaches for Phil. His akinetic mutism symptoms improved significantly once we were able to identify a neurological etiology for observed behaviors, to determine appropriate goals and to use evidence-based practice for effective therapy.
As a four-month resident of our facility, Phil continues to progress toward independence in execution of ADLs. He has graduated from requiring two-person transfer assist to the independent use of a walker and improved independence in bowel and bladder care so he can return home.