By Jamie Funk, Therapy Recruiting Resource
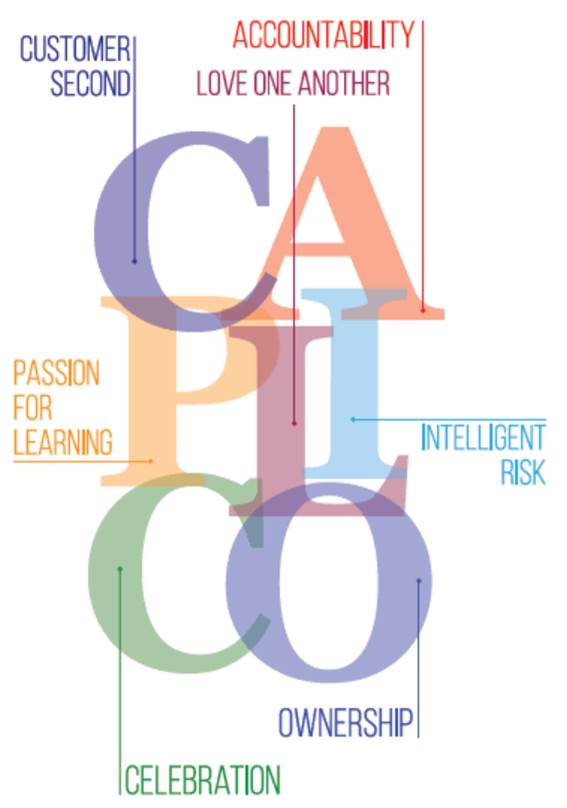
Dennis Baloy is one of our more recent additions to the Ensign affiliated therapy leadership team. As the Director of Rehabilitation at St. Elizabeth Healthcare & Rehabilitation Center, Dennis immediately recognized our unique culture: “I just want everyone to know how lucky I feel to be part of this wonderful organization that truly embodies the value of Customer Second, where we as therapists and employees are celebrated, valued and appreciated. I am even more humbled to be surrounded by really bright, talented and passionate leaders. Everyone is so inspiring in their unique ways. Collectively, this is what truly sets us apart!”
Dennis has been a therapist for 15 years and a Director of Rehabilitation for the past eight years. He graduated with his Bachelor of Science in Occupational Therapy in the Philippines and later completed his Clinical Doctorate in Occupational Therapy with Geriatric Certification in the United States. As a child, Dennis always wanted to become a doctor and thought therapy might be a stepping stone to that career. However, as he immersed himself in his first OT internship, Dennis realized that OT was it for him — a career that would allow him to care for others, be creative and be human. Dennis has two brothers who are his biggest inspiration and mentors: Paul and Kirby. “They are the biggest reasons why I am where I am with my career,” Dennis says.
During the Ensign transition at St. Elizabeth, Dennis saw that culture was a top priority. “It was refreshing to see how involved all employees are in the facility. No longer does each department feel separate from one another. Every staff member is valued equally and has a voice. The support from our resources and Service Center is always present when you need it — this was definitely a big change in mindset for me coming from a corporate hierarchical structure,” Dennis remembers.
Dennis says that his biggest challenge has been being new in our company, new in his role and then having relentless COVID outbreaks in the community to deal with. “It has been stressful at times, but for the most part it is just a big challenge that I am willing to face. I feel like I don’t know a lot of things and that I still need to learn a lot of technical items, but I am excited to listen and grow. There is a huge sense of fulfillment if you know you can be of service to others and spread positive and enriching influence.”
Dennis has shown himself to be a wonderful leader. He loves being able to see his colleagues go out on their own and feel like they can do their jobs well because they feel valued, appreciated, empowered and loved. “Nothing beats the feeling of knowing that they love coming to work, they love their patients and their profession, and they can provide for their families and be themselves,” Dennis explains, “My favorite core value is Love One Another. Love at its core is selfless — the moment we think less of ourselves and more of the betterment of others. This allows us to build a community of trust, and this trust allows us to better serve our facility, our patients and our community.”
Dennis finds mentors throughout his facility. “I see everyone in my facility as my mentor,” he says. “I learn so much from each of the department heads and especially my administrator and DON — they all have strong attributes that complement each other and the whole facility.” Dennis also loves his nursing team and treats them like family. He has been able to build strong relationships with nursing through honest and genuine communication.
In his off-work hours, Dennis is passionate about photography and videography. He owns his own company, and pre-COVID, was very busy providing those services at weddings and other events. He still spends a lot of time taking photos and creating videos for fun. Dennis has also fallen in love with the world of triathlons and has set a goal to complete an Ironman competition in 2021. Favorite movies include “Braveheart,” “50 First Dates,” “Memento,” “Crash,” “Into the Wild” and a variety of Disney movies that he watches with his family.
As for the future, Dennis is focused on both family and work. “I would just love to see my daughter grow to be a nice kid — a good, smiling and happy kid. I want her to get to be who she wants to be and be happy doing that and being helpful to others. I have a goal to spend more quality time with my wife at home and hopefully some future trips together.” Dennis is looking forward to seeing his facility GROW. His goal is to serve more residents with inpatient and outpatient services and be recognized in the community as a skilled nursing facility that provides excellent clinical care that is warm, loving and inviting. He would also love to help spread this to the other Ensign affiliates in his area.
It always seems like something magical and wonderful has happened when a great therapist finds a great place to work and grow. Magic is definitely happening at St. Elizabeth!
 By Shelby Donahoo, Therapy Resource, Tucson, AZ
By Shelby Donahoo, Therapy Resource, Tucson, AZ

 This is our first group treatment since October, which is when we went into full lock-down, outbreak mode. It was organized by two of the most compassionate therapists I know, Emily White, PTA, and Wendy Garrison, OTA. The residents had a blast!
This is our first group treatment since October, which is when we went into full lock-down, outbreak mode. It was organized by two of the most compassionate therapists I know, Emily White, PTA, and Wendy Garrison, OTA. The residents had a blast! This is Ron; he was in a catastrophic car accident in 2019, which brought him to us. He received prosthetic training and was set to go home in early November, when he tested positive for COVID. Plans to DC home were postponed, but he made it, and has made it back home to Nebraska.
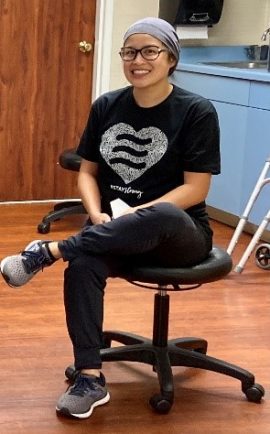
This is Ron; he was in a catastrophic car accident in 2019, which brought him to us. He received prosthetic training and was set to go home in early November, when he tested positive for COVID. Plans to DC home were postponed, but he made it, and has made it back home to Nebraska. This is Jessica, the Clinical lead and head cheerleader for team Ron. We all cried like babies when he finally went home.
This is Jessica, the Clinical lead and head cheerleader for team Ron. We all cried like babies when he finally went home. As a compromised patient, Glenna should not have survived, according to all our knowledge of the virus, but she did. What a happy day it was to move her off of the COVID wing back to her own room.
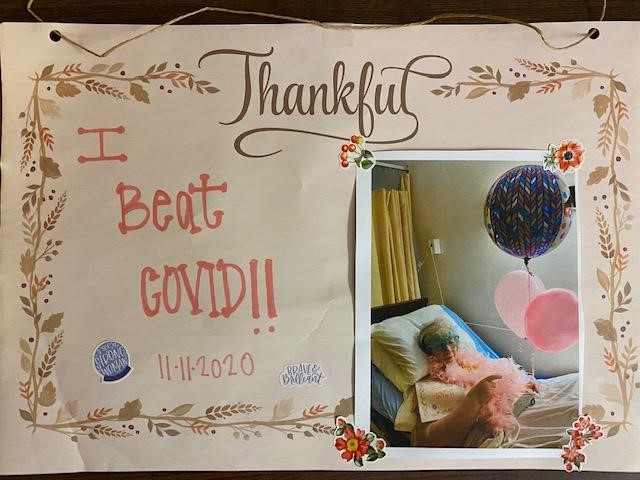
As a compromised patient, Glenna should not have survived, according to all our knowledge of the virus, but she did. What a happy day it was to move her off of the COVID wing back to her own room. This was our very first survivor. She didn’t even know she was sick and was happily confused about all the fuss we were making over her. We are all truly thankful for the opportunity to celebrate with her. (photo of thankful I beat COVID)
This was our very first survivor. She didn’t even know she was sick and was happily confused about all the fuss we were making over her. We are all truly thankful for the opportunity to celebrate with her. (photo of thankful I beat COVID)




 Denise Del Cano, COTA, ADOR, has dedicated her career in The Hills Post Acute. An alumnus of Santa Ana College, she earned her associate’s degree in Occupational Therapy Assistant 12 years ago and has been with the facility since then. She was promoted to Assistant Director of Rehab last year and completed the DORITO program this year. Denise did her internship here at The Hills. She was supervised by Vonda Gaier, COTA, who then became her colleague. She is a Filipino American born in Los Angeles, California, the eldest of five and a loving mother to her 16-year-old daughter, Elizabeth. Interestingly, Denise was introduced to the field of therapy when her daughter received therapy for several years. Denise saw the importance and relevance of Occupational Therapy and has been an advocate ever since.
Denise Del Cano, COTA, ADOR, has dedicated her career in The Hills Post Acute. An alumnus of Santa Ana College, she earned her associate’s degree in Occupational Therapy Assistant 12 years ago and has been with the facility since then. She was promoted to Assistant Director of Rehab last year and completed the DORITO program this year. Denise did her internship here at The Hills. She was supervised by Vonda Gaier, COTA, who then became her colleague. She is a Filipino American born in Los Angeles, California, the eldest of five and a loving mother to her 16-year-old daughter, Elizabeth. Interestingly, Denise was introduced to the field of therapy when her daughter received therapy for several years. Denise saw the importance and relevance of Occupational Therapy and has been an advocate ever since.
 Out of the blue, Michael and Mitch stepped in, offering a memorial service to honor and remember those we lost over the past several months. They set everything up, even though I knew their services were widely needed during that time. I can honestly tell you we cried and held each other a lot during that time. We were grateful for Emblem’s offering and kindness when we needed it the most. One of them brought a grill on wheels (not sure whose it was, but it is pretty sweet) and cooked up burgers and hot dogs for all the staff over a four-hour period. It was hot outside, but Michael didn’t seem to mind it — it was 115 that day.
Out of the blue, Michael and Mitch stepped in, offering a memorial service to honor and remember those we lost over the past several months. They set everything up, even though I knew their services were widely needed during that time. I can honestly tell you we cried and held each other a lot during that time. We were grateful for Emblem’s offering and kindness when we needed it the most. One of them brought a grill on wheels (not sure whose it was, but it is pretty sweet) and cooked up burgers and hot dogs for all the staff over a four-hour period. It was hot outside, but Michael didn’t seem to mind it — it was 115 that day. 