 Congratulations to our newest SPARC Award Winner, Hannah Ruth Downing, SLP Student at Sacramento State University, Grad Date 5/19/2019
Congratulations to our newest SPARC Award Winner, Hannah Ruth Downing, SLP Student at Sacramento State University, Grad Date 5/19/2019
Read her Winning Essay Here:
“What do you want to be when you grow up?” is the question I was continually asked as a child. Being raised in the Filipino culture, one is expected to become a nurse, doctor, or have almost any job relating to the medical field, but this did not seem like something I wanted to do. From a young age I enjoyed the idea of becoming a teacher. As I grew older I tutored elementary students at a local middle school, and there my ardor for helping kids increased. The thought of becoming a teacher continued to linger in my mind, but the voices of others encouraged me to choose otherwise. Going into college, I chose to pursue occupational therapy due to the fact that it was in the medical field, and I could specialize in pediatrics. However, I quickly realized that occupational therapy was not the career choice that suited me best. I then stumbled upon speech pathology. This career field had both aspects that I was looking for, teaching kids while being in the medical field. The classes I began to take and the volunteer work that coincided, sparked my interest.
Having finished my first two semesters in the communication sciences and disorders major, I was taught the basics such as the anatomy that is used for speech and swallow, language disorders in children, how effects to the brain can disrupt the language process, and various other topics. I soaked up the majority of the information given to me by my professors and I enjoyed learning everything, but by putting the knowledge I had obtained, over the two semesters into practice, I was enabled to truly comprehend the things that were taught to me.
During the first two years in college I was a childcare attendant at California Fitness. I was able to observe and interact with typically developing children, and with the knowledge I held at the time, I was able to distinguish kids that incorrectly produce sounds that were typical for their age and others who could not. This was the first encounter where I was able to practice what I had learned. This aroused my desire to learn more in order to implement the information I was attaining, so I decided that I needed more exposure to the field that I was working towards. During my third year, I got hired at Genesis Behavior Center as a behavioral therapist working with children with autism. This job has allowed me to apply a lot of the information about autism that was taught by my professors because a lot of the clients on an SLPs case load are on the spectrum. The most impactful thing that I have obtained, as well as what has driven me to learn more from being a behavioral therapist, is the struggle of communication that someone with autism faces. As a behavioral therapist, I have to train my clients how to communicate their emotions in the most effective way. In training a child with autism, how to do this can be complicated and it can take weeks, months, or even years to accomplish. However, when the child finally understands that when they are mad the inappropriate thing to do is throw a chair across the room, and instead they can simply state that they are mad and take some deep breaths to calm down, this is the moment that brings me so much joy. I have learned that communication is extremely important, and when communication is hindered, by a developmental disorder like autism or aphasia from a stroke, it can cause a copious amount of stress on the person with a disability as well as the people around them.
Working at Genesis reaffirmed my love for working with children, and although my passion for helping kids had increased, I still needed to gain experience by working with adults. I began getting involved with several organizations such as Elk Grove Adult Community Training (EGACT) and Training Toward Self Reliance (TTSR) where they both work with adults with developmental disabilities such as Down’s Syndrome, cerebral palsy, or autism, Head Trauma Support Program (HTSP) where they work with clients who have had a traumatic brain injury, and lastly stroke support group. Volunteering at these organizations was an immense revelation that left me heartbroken. There were two paramount concepts that I gained from my experience, first was the fact that kids grow up. I knew that kids obviously grow up, but I forgot that even though they get older their disabilities do not disappear. There is so much focus on early intervention, which is not a bad thing, but people often forget that adults with disabilities still need guidance and assistance. I was so happy to see day centers like EGACT and TTSR assist adults with disabilities go to and interact with each other as well as guide them so that they can continue to be a part of society regardless of their condition.
The second concept was the fact that before the patients had a stroke or TBI, they lived functionally. When going to HTSP meetings I noticed that a lot of the clients had tattoos. In order to get those tattoos they had to have the ability to make the executive decision to get something that would be permanently on their body, however, when you see them now they cannot even form a sentence, let alone a word. I realized that a lot people that encounter patients with TBIs or strokes were treating them as a person with a disability, and not just as a person. We often forget they used to have normal lives and were capable of accomplishing daily tasks themselves, and that they are just working to get back to what they remember as normal. One of the patients at the stroke support group meeting stated that, “It was like tracing out your ABC on the wide rule paper like you were in kindergarten again, but in kindergarten I probably did it better. I have to learn everything over like I’m a child.” This statement impacted the way I saw patients that had gone through a stroke or TBI. It made me realize how frustrating ever day must be for them, and going to school to potentially become someone that could help them try to get back to living functionally really encouraged me. Even though my passion is working with children, volunteering at these organizations has not only opened my eyes to many misunderstood concepts, but it has also driven me to want to understand and learn more about working with adults.
Overall, the classes I have taken for communication sciences and disorders, have aided me when I am volunteering. It allowed me to understand the absence of pragmatic skills in kids with autism, and the many different aphasias one can experience after enduring a stroke. I can easily see and pinpoint things I am learning in class to what I experience as I work and volunteer. I am aware that I still have so much to learn because even though with all the knowledge I have obtained, I continuously ask myself questions when I encounter certain situations. These questions can only be answered as I learn more, which has driven me to want to continue in my education. This scholarship money will allow me to further this desire of learning in order to gain more experience, enabling me to treat my future clients with the utmost excellent care they deserve.


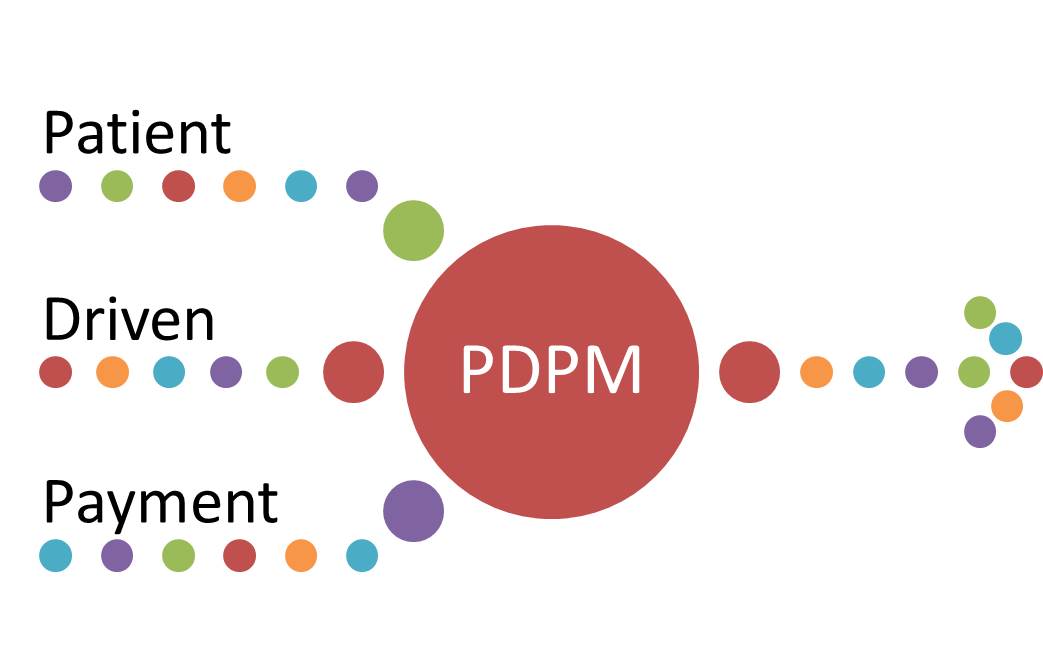
 The proposed rule Fiscal Year 2019 has been considered by many to be the most anticipated rule proposal since the introduction of the Medicare Prospective Payment System in 1998. The NPRM was released to the public on Friday, April 27, 2018, and introduced us to a new payment model entitled, the Patient Driven Payment Model (PDPM), which is suggested in the rule to become effective in October 2019.
The proposed rule Fiscal Year 2019 has been considered by many to be the most anticipated rule proposal since the introduction of the Medicare Prospective Payment System in 1998. The NPRM was released to the public on Friday, April 27, 2018, and introduced us to a new payment model entitled, the Patient Driven Payment Model (PDPM), which is suggested in the rule to become effective in October 2019.

 Speech, in particular, utilizes pitch, rhythm, and timbre—all elements of music (Smith, 2011). Because of these significant areas of overlap, music and speech carry a natural relationship. But most obviously, music moves people. The right song can bring back the fondest of memories. Hearing the sweet sounds of the right melody can turn a hopeless situation into hopeful. Singing in particular, reverberates the music inside one’s body. In these ways, I hope to use music to spark energy, motivation, and happiness into the lives of my patients.
Speech, in particular, utilizes pitch, rhythm, and timbre—all elements of music (Smith, 2011). Because of these significant areas of overlap, music and speech carry a natural relationship. But most obviously, music moves people. The right song can bring back the fondest of memories. Hearing the sweet sounds of the right melody can turn a hopeless situation into hopeful. Singing in particular, reverberates the music inside one’s body. In these ways, I hope to use music to spark energy, motivation, and happiness into the lives of my patients.




 The North Mountain Therapy Department specializes in Pulmonary Rehab, encouraging a multi-disciplinary approach to meet our respiratory patients’ goals of being decannulated, which typically is dependent upon the patient’s ability to return to a regular diet. In an effort to contribute to the greater independence of our patients, the Therapy Department created the SPOT (Speech Pathology Occupational Therapy), a holistic approach to a specialized dining experience to facilitate independence with safe swallow techniques and self-feeding.
The North Mountain Therapy Department specializes in Pulmonary Rehab, encouraging a multi-disciplinary approach to meet our respiratory patients’ goals of being decannulated, which typically is dependent upon the patient’s ability to return to a regular diet. In an effort to contribute to the greater independence of our patients, the Therapy Department created the SPOT (Speech Pathology Occupational Therapy), a holistic approach to a specialized dining experience to facilitate independence with safe swallow techniques and self-feeding.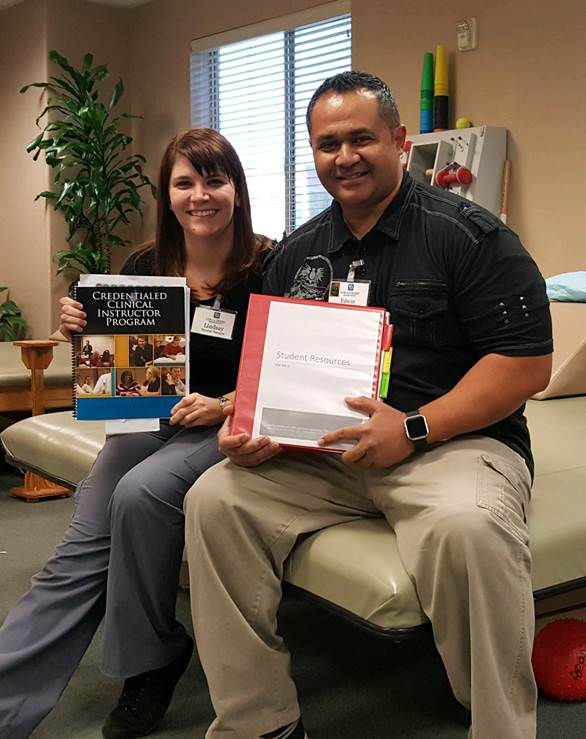
 What was initially simply a continuing education experience for two therapists has inspired a brand-new program here at Coral Desert Rehabilitation. Recently, a Coral Desert physical therapist, Lindsay Rankin, and a physical therapist assistant, Edwin Stevenson, attended a course to become credentialed clinical instructors. They both enjoy having students, so they were excited to go. After attending the course, they came back with a desire not only to improve their own abilities, but also to help revamp the student program at Coral Desert.
What was initially simply a continuing education experience for two therapists has inspired a brand-new program here at Coral Desert Rehabilitation. Recently, a Coral Desert physical therapist, Lindsay Rankin, and a physical therapist assistant, Edwin Stevenson, attended a course to become credentialed clinical instructors. They both enjoy having students, so they were excited to go. After attending the course, they came back with a desire not only to improve their own abilities, but also to help revamp the student program at Coral Desert.
