 We congratulate Avenlea Gamble and Kellye McKee, our new scholarship winners for this quarter! Read their awesome essays below:
We congratulate Avenlea Gamble and Kellye McKee, our new scholarship winners for this quarter! Read their awesome essays below:
Avenlea Gamble, SLP Student at University of the Pacific, Stockton, CA, Grad Date: December, 2017
The opportunity I was afforded as a student clinician at the Pacific Speech, Hearing and Language Center was a formative experience to my education and cemented my interest in serving the adult population in the field of speech/language pathology. University of the Pacific has provided me the ability to work across a lifetime of demographics during the short time I’ve been here, but my favored clinical experience was within the adult clinic. There I was able to work with individuals who truly inspired me as a clinician. I believe the most rewarding aspect of working with an adult demographic is that you are returning a voice or supporting the ability to communicate with a group of individuals who could freely communicate prior to the incident or diagnosis that changed their lives.
Reading a textbook provides a limited academic view into the disorders and the individuals in which we will see these disorders realized. Actually working in the clinic brought a humanity to our field that a classroom can’t provide, and challenged me as a developing clinician to take static information and apply it to the improvement of my clients’ lives. I was working with individuals who were struggling or lost their jobs because of their communication problems; clients who had given up on past times or lifelong interests because of the deficits they now faced; or even people who couldn’t tell their family that they loved them.
I was raised in skilled nursing facilities, visiting one when I was three days old and returning regularly since then. My mother began working in the local skilled nursing facility in our rural hometown of Willits, California, when she was 17, and I started working there when I was 16. I worked under the social services department as a Care Partner, a position in which I was tasked with providing psychosocial support to the residents. One aspect of my job was attending residents’ appointments with them, and I began regularly taking one resident to his speech-language pathology appointments at the local hospital. Watching the clinician work with my resident lead to the realization that I could see myself in that position, fulfilling that role of returning and supporting the communicative abilities of my community members, and seven years later, here I am at University of the Pacific, in my final year of schooling to do just that.
I was also employed in the social services, dietary, human resources, compliance, and administrative departments at the nursing facility. My experience in the adult clinic at Pacific, as well as the different departments of the skilled nursing facility, have given me a unique and collaborative insight into the needs of the adult and geriatric populations that speech-language pathologists often serve. I want to improve the quality of life of individuals with dysphagia using the dietary and speech-language pathology experience I have gained, as well as bolster the cognitive-linguistic support for individuals with different neurological disorders or disorders secondary to brain injury or cardiovascular injuries. My personal goals lie in dementia capable care, aphasia therapy with couples or in the group setting, and stronger collaboration between the dietary staff, registered dietician, and SLP to provide a better quality of life for individuals on specialized or thickened diets. The adult and geriatric population are a precious resource to us because of their life experience and wisdom, and they must be respected and provided the highest quality of life they may receive during the golden years towards the end of their lives.
I supported clients who presented with different aphasias, voice disorders, dysarthria, apraxia, and a laryngectomy. A chart review gives the clinician a very limited view into the client – every client is incredibly unique, and no two people with aphasia present the same. It’s a continuous challenge which allows clinicians to continue growing and learning throughout their careers.
My combined experience at the skilled nursing facility and adult clinic at Pacific have fostered an empathy and compassion in me for the adult population that I will carry with me throughout my career and life. As long as I have the ability to serve, I have a duty to support the communication needs of this population and my community as a whole using my education and clinical experiences.
I come from a small community, a town of about 4800 individuals, so when a patient passes through my door, they are not a stranger. They are a community member, a friend, a member of the family. My wonderful education, clinical experience, and lifelong growth within skilled nursing facilities will allow me to be that spark for my patients, because serving this population has been what has defined my life thus far, and what gives me the deepest satisfaction that I have known.
Kellye McKee, PT Student at Rocky Mountain University of Health Professions, Provo, UT, Grad Date: December 2017
Go across the floor leading with your bones. Come back by moving your muscles. The words of my college dance professor resonated through my head as I attempted to move my body forward, leading with my pelvis and allowing the rest of my body to follow. Unbeknownst to me, that class and its concentration on dance anatomy would determine the focus of my college education. Ultimately, it sparked my passion for the human body and how it moves and works, leading me to pursue a career in physical therapy.
Dance allows me to comprehensively explore my body and the intricacies of its movements. Performing as a professional dancer from 2007 until 2015 gave me the opportunity to express my love and knowledge of dance. As a performer, I love envisioning and understanding the muscles, ligaments, and tendons that allow me to twist, bend, and leap across the stage. That connection to, and awareness of, my own body has facilitated a passion for kinesiology and anatomy, as well as a deeper understanding of how the body heals and recovers from injuries. After thoroughly enjoying a human anatomy course, I began exploring career paths centered on the human body and health care. This is when I discovered physical therapy.
My strongest draw to the profession of physical therapy was the opportunity to use my education and training to spark a passion in my patients and to empower each one. When patients gain insight into their diagnoses and deficits, they can use that education to help themselves improve and heal. Knowledge is power, and knowledge concerning one’s own body sparks a lifelong motivation to continue working toward a healthy body. Another passion of mine that is rooted in body awareness is working as an instructor for The Dailey Method barre exercise class. Being a TDM instructor has given me the opportunity to help people build strength and flexibility through education, encouragement, and hands-on adjustments.
The Dailey Method approach is centered around proper body alignment and controlled, non-impact movement that engages the body deeply. It has been rewarding to help people reach their physical and mental goals. That lifelong love of learning has contributed to each client’s well being. Of course, people coming on their own to The Dailey Method classes are motivated in a different way than some physical therapy patients, including patients in a skilled nursing facility. Sparking a patient’s desire to improve requires flexibility and a positive attitude, as well as knowledge and training in the importance of physical activity.
My appreciation for the human body has grown during my eight-year career as a professional white water raft guide. Being a raft guide provides me with extensive experience working with a diverse group of customers, each with his or her own individual needs, thoughts, and personalities. Rafting gives me the opportunity to accept and appreciate diversity as well as provide an environment for my interpersonal skills to flourish. These skills are essential for working as a physical therapist. My ability to communicate with a wide range of people, combined with my desire to facilitate healing, allows me to work collaboratively and effectively with patients and other health professionals. Being a raft guide has to do with safety first, and providing a safe trip often has much to do with the guide’s ability to motivate customers to dig in, work hard, and paddle together as a team. These skills are certainly transferable to the world of physical therapy. Creating a safe run down rapids require setting goals and planning how to achieve that success.
Creating success for a patient involves their help in setting their own goals and their involvement in planning for their own long-term and lasting success. Freedom to spend more time with each patient, beyond corporate limitations, would create a more patient-centered approach. Having that freedom was would allow the flexibility and time to try different evidence-based approaches. My physical therapy career choice was further affirmed at the beginning of the 2014 rafting season. I had begun the season with back pain that was not responsive to my usual stretching and strengthening regimen. I had also begun seeing a chiropractor and acupuncturist but had little relief. One of the guests on my first rafting trip of the season happened to be a physical therapist and was more than happy to help me. She explained what she believed was causing the pain and recommended several daily exercises. She also listed motions and movements that I should try to avoid, as these motions would have a negative impact on my back. I followed her advice and in just a few weeks I was feeling better than I had in months. It was inspiring to discover that a few physical therapy exercises and stretches could make such an impact. I strive to pass along that same knowledge: understanding and respect for the human body. I also want to be able to help others with their physical ailments the way this therapist had helped me.
As a student of physical therapy, I learned so much about the human body, what it is made up of, how it works and why, and what can go wrong. I found this education fascinating, and I am inspired to learn more everyday. Now that I am an intern and able to spend time with patients, I love to pass on my knowledge and hope to inspire everyone I encounter. I have worked with many patients who were unmotivated to participate in physical therapy. One that stands out was a male in his 30s who had been in a bad car accident ten years prior and had been living with severe back pain ever since. He was prepared to spend the rest of his life with limited activity and in severe and constant pain, but he decided to give physical therapy a chance. He did not particularly enjoy the first few treatments, but he was compliant with the home exercise program I prescribed, and he continued to come in for his appointments. After three treatment sessions, he reported a decrease in back pain, and by the fifth visit claimed to feel the best he had felt in ten years. By the end of our visits, the patient was able to participate in every activity that his pain levels had kept him from enjoying. He was so thankful for the help and education that he had received. I was inspired by the improvements he was able to make, and his profound appreciation for the successful treatment resonated deeply with me. This gratitude will serve well as a reminder throughout my career as a physical therapist that even the most unmotivated patients can be helped.
Witnessing firsthand the interactions between Ensign physical therapists and their patients, I am continually inspired by the communications I witness, the improvements the patients make through therapy, and the compassion shown by the physical therapists. Using my background as a professional dancer, raft guide, and as an instructor at The Dailey Method, it is my goal is to inspire each and every physical therapy patient I have the privilege to treat.
 Clients with dementia living in skilled nursing facilities have occupational needs that are often unmet. Individualized care approaches and engagement in meaningful activities are effective non-pharmacologic approaches to dementia care. However, they are infrequently implemented in SNFs, and patients with dementia are often medicated with antipsychotic medications to manage behavioral symptoms related to dementia.
Clients with dementia living in skilled nursing facilities have occupational needs that are often unmet. Individualized care approaches and engagement in meaningful activities are effective non-pharmacologic approaches to dementia care. However, they are infrequently implemented in SNFs, and patients with dementia are often medicated with antipsychotic medications to manage behavioral symptoms related to dementia.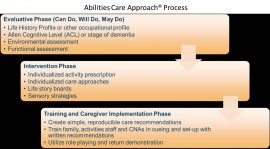



 After noticing a recent increase in falls and fall-related injuries at our building, we wanted to better understand the mechanisms of the falls and implement a comprehensive, interdisciplinary fall prevention program.
After noticing a recent increase in falls and fall-related injuries at our building, we wanted to better understand the mechanisms of the falls and implement a comprehensive, interdisciplinary fall prevention program.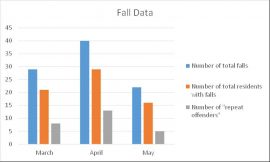

 As healthcare professionals, we often discuss dementia in the context of various stages, that is, how far a person’s dementia has progressed. Sometimes, we’ll define a person’s stage simply as early-stage, middle-stage or late-stage; however, to be more exact, we use the Global Deterioration Scale (GDS), which assigns seven different dementia stages based on the degree of cognitive decline.
As healthcare professionals, we often discuss dementia in the context of various stages, that is, how far a person’s dementia has progressed. Sometimes, we’ll define a person’s stage simply as early-stage, middle-stage or late-stage; however, to be more exact, we use the Global Deterioration Scale (GDS), which assigns seven different dementia stages based on the degree of cognitive decline. Last year, Ensign therapists were introduced to a new balance pad system called the Sanddune Stepper. It is said to have significant effects on improving proprioception and ankle strategy in patients with a neurological diagnosis.
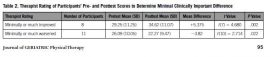
Last year, Ensign therapists were introduced to a new balance pad system called the Sanddune Stepper. It is said to have significant effects on improving proprioception and ankle strategy in patients with a neurological diagnosis.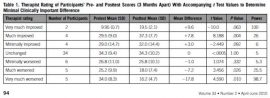

 We congratulate Avenlea Gamble and Kellye McKee, our new scholarship winners for this quarter! Read their awesome essays below:
We congratulate Avenlea Gamble and Kellye McKee, our new scholarship winners for this quarter! Read their awesome essays below:
 Did you know we have an exciting new opportunity with Ensign? We are starting our very own internal travel program! What? Yes, we’ll have our own internal team of travelers who will go and serve in any of our communities. We have been asked by several DORs and EDs for the past several years when we could start something like this … well, here we go!
Did you know we have an exciting new opportunity with Ensign? We are starting our very own internal travel program! What? Yes, we’ll have our own internal team of travelers who will go and serve in any of our communities. We have been asked by several DORs and EDs for the past several years when we could start something like this … well, here we go!
