
Here’s what we’re all about!


We hosted the CE at our Legend West Houston facility. Nursing and rehab must be cohesive to a have a strong contracture management program. I sent an email out to our DONs and they welcomed the idea of including our RNAs. John even provided them with certificates. They loved it.
Thank you to those who were able to make it to the Contracture Management Course on Saturday. We had a great turnout from several of your therapists/assistants as well as your RNAs. The course speakers had an opportunity to visit the Katy and West Houston facilities, the day before the course, and provide face-to-face assistance. Tawaine and Brittany gave very positive reviews and stated that several patients were identified for therapy services that were previously overlooked.
Below, you will find the names and contact information of the speakers. Both are available to provide telemedicine support. What does that mean to you? If you have a patient you are considering for an orthotic and/or you need recommendations on the best splints, they are available by phone or FaceTime to provide guidance. They are also available to assist with verification of orthotics (especially for our managed care part B residents). All you need to do is send them the patient’s face sheet, and they will take care of the rest. Please take advantage of this available resource. We have several patients within our facilities with contractures, and our obligation is to provide the best quality of care available. Special Ensign pricing is available to us.
OCSI: Ongoing Care Solutions, Inc.
John Kenney: 949-702-2828 neuroflexjk@gmail.com
Regan Ponto: 970-978-1284 regancap@msn.com
Submitted by Kai Williams, Therapy Resource, Texas
 Beth Brewer, OTR/ADOR at Legend Oaks Katy, is known to most of us by her acquired moniker, MacGyver. What she creates with “a little bit” of duct tape, PVC pipe and pool noodles is magical! So when we decided to make dementia care one of our focal clinical programs, it came as no surprise that she would create something great.
Beth Brewer, OTR/ADOR at Legend Oaks Katy, is known to most of us by her acquired moniker, MacGyver. What she creates with “a little bit” of duct tape, PVC pipe and pool noodles is magical! So when we decided to make dementia care one of our focal clinical programs, it came as no surprise that she would create something great.
This is when the Dementia Care Activity Box was born. Using guidelines from Teepa Snow’s The Gems®: Brain Change Model, Beth created Dementia Care Activity Boxes based on various dementia characteristics (gems). All facility staff have received an initial in-service/training on the purpose and use of the activity boxes, which are accompanied by a matching resource binder with descriptors for each gem; dialogue cheat sheets to engage residents in eating, bathing and dressing tasks; as well as general information about dementia. In addition to the activity boxes, Beth also recently piloted a four-resident Dementia Feeding Program using red plates and bowls to increase self-feeding and po intake. So far, we’ve seen a 10 percent to 25 percent increase in po intake depending on the resident’s level of dementia.
Our Dementia Care Program is in its infancy stages; however, with “MacGyver” Beth at the helm, I know that our residents are destined for greatness!
Submitted by Tawaine Vigers, DOR, Legend Oaks of Katy, TX
“Employees want to know why they have to produce and deliver services by using certain methods. To be good at holding your staff accountable, you must be good at teaching. Teach about the consequences.” — Crucial Accountability
Did you know that poor documentation quality has a bigger financial impact than productivity does? It’s true! In general, while you save $0.02 for every 1 percent productivity increase, billing minutes pulled out during an audit will have a much greater financial loss:
RUC x 14 days (647.94/day = $9,071.16)
RVC x 14 days ($555.85/day = $7,781.90)
In conclusion, one billing minute removed due to unskilled documentation could result in a $1,289.26 loss.
DOR Role
What is the role of the DOR? We define it as follows:
UR prep and care plans must:
Teach the Why
In order to hold staff accountable for skilled documentation, it’s important to engage your team in dynamic thinking about the “why” behind what they do. That is, educate them as to why quality documentation is important, as it not only reflects their clinical skill, but also ensures we can be billed for services and therefore has a financial impact. Finally, provide lists of commonly used skilled terms descriptive of therapists’ actions.
MSCA Data
Skilled documentation is a critical part of our systems at Granite Creek Health and Rehabilitation. By implementing training in this area, we saw an improvement in the MSCA therapy score and a decrease in the financial error rate:
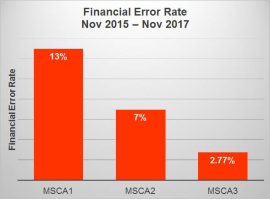
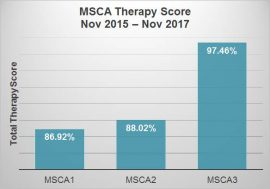
By Larissa Osio, DOR, MS OTR/L, Granite Creek Health and Rehabilitation, Prescott, AZ
View full poster here: Accountability and Skilled Documentation -Granite Creek
 At Grand Terrace Rehabilitation and Nursing, we have implemented an Oral Hygiene Program with great success for residents. The purpose of the program is multifold:
At Grand Terrace Rehabilitation and Nursing, we have implemented an Oral Hygiene Program with great success for residents. The purpose of the program is multifold:
Methods
Results
As a result of the program, our residents have gained an improved quality of life and decreased caregiver dependence. We have increased CNA productivity due to residents requiring less assistance, while also decreasing hospitalizations due to medical complications associated with poor oral care. In addition, we have seen increased interdisciplinary team communication.
The oral hygiene program has benefited residents, caregivers, therapy and the facility. Not only have we boosted awareness of the importance of providing good oral care, but we have also enhanced residents’ self-efficacy.
By Grand Terrace Rehabilitation and Nursing, Therapy Department, McAllen, TX
 Our skilled population has gradually shifted from traditional Medicare Part A to Managed Care Part A. Therefore, our treatment focus has had to shift as well. We are no longer focusing on progressing to prior level of function, but rather progressing to next level of care.
Our skilled population has gradually shifted from traditional Medicare Part A to Managed Care Part A. Therefore, our treatment focus has had to shift as well. We are no longer focusing on progressing to prior level of function, but rather progressing to next level of care.
Methods
With the goal of reducing the length of stay, we determined that we needed to aggressively treat at onset of stay. To jumpstart our therapists and create a routine for the patients, we implemented the following days:
Results
Since the implementation of our protocol, the length of stay has decreased on our managed care from 18.4 days to 15.6 days. Reviewing the length of stay of our Medicare A patients, it has dropped from 30 days to 27.9 days. During the course of review, which was a six-month period, we had 196 Managed Care patients and 58 Medicare A patients.
Conclusion
Our goals include the following:
By Andy Cisneros, PTA, Therapy Program Manager, Legend Oaks, West San Antonio, TX
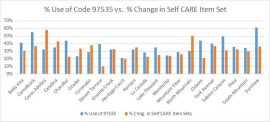
At Mountain View Care Center, we questioned whether there is a correlation between the amount of activities of daily living (ADLs) the occupational therapy staff has been providing to patients with changes in their’ functional level upon discharge. We chose to compare this by analyzing the percentage of ADLs billed in the facility with the change in CARE item set from admission to discharge.
Methods
We gathered Optima reports from all Bandera facilities to determine service code usage of self CARE ADLs (97535) as a percentage of total billable services for a three-month time period. Functional Outcomes report containing the change in OT Self CARE item assessment was obtained for the same three-month time period. These two reports were analyzed to determine if there was a correlation between the two sets of data.
Results
The amount of billing of 97350 seemed to equate with the amount of change in CARE. However, upon closer statistical analysis, this was not found to be the case. There was no correlation found between use of ADL billing code (97535) and improvement in CARE item set. Billing of the code 97110 had a negative correlation with the improvement in ADL scores.
Data
Conclusion
We concluded the following:
In the future, we’d like to further our analysis by performing a study using a change in ADL levels instead of CARE to decrease concerns about CARE not being an accurate measure of improvement. Furthermore, after educating the staff on the increased use of ADLS as a modality, we’d like to perform the same analysis to determine if there was an increase in CARE item assessment as a result of increased ADL usage.
By Tonya Haynes, PT, DOR, Mountain View Care Center, Tucson, AZ
 At Northeast Nursing and Rehabilitation, we cared for a 77-year-old white male who had been recently hospitalized for acute cholecystitis. His PMH included CAD, a pacemaker, cardiac stents, HTN and COPD. The patient presented with a variety of problems, including debility, decreased ADLs, poor static/dynamic and sitting/standing balance, decreased mobility, decreased aerobic endurance and breathing abilities, and poor phonation.The patient also had decreased breath control, able to produce only three words without taking a breath. He required constant oxygen and had little diaphragmatic breathing, possibly related to the secondary effects of COPD.
At Northeast Nursing and Rehabilitation, we cared for a 77-year-old white male who had been recently hospitalized for acute cholecystitis. His PMH included CAD, a pacemaker, cardiac stents, HTN and COPD. The patient presented with a variety of problems, including debility, decreased ADLs, poor static/dynamic and sitting/standing balance, decreased mobility, decreased aerobic endurance and breathing abilities, and poor phonation.The patient also had decreased breath control, able to produce only three words without taking a breath. He required constant oxygen and had little diaphragmatic breathing, possibly related to the secondary effects of COPD.
Prior Level of Function
Prior to admission, the patient was ambulatory with a cane for household distances. He was I with ADLs, bed mobility and toileting, as well as I with dressing and hygiene/grooming. He consumed a regular diet, had good aerobic condition and did not require oxygen.
Interventions
We employed several strategies to help the patient, including physical, occupational and speech therapy interventions. For example:
Outcomes
As as result of our interventions, the patient showed marked improvement in several areas, including functional gait distances with use of a cane, improved dexterity and fine motor control, LB dressing, toileting and more. His phonation improved, and the patient did not require oxygen at home. Ultimately, the patient was able to return home with the support of his family and thanks to the combined efforts of our therapy teams.
By Rochelle Lefton, MA, OTR; Michelle Scribner, MSLP; Heather Cox, DPT; Susan Garcia, COTA; Jesusa Herrera, PTA, Northeast Nursing and Rehabilitation, San Antonio, TX
Patient Centered Care isn’t just taking good care of our patients. It is a holistic philosophy of including the patient and their family members in as many decisions and system/facility improvements as possible. It means offering choices whenever possible, thereby giving our elders more control over their lives.
This approach may include asking for their input on anything from what kind of furniture they would like to replace the old furniture in the front lobby, to what we should ask them on a discharge survey, to simply when they would like to go to bed at night. We are still in our infancy with implementing this philosophy, but here is what we have accomplished thus far:
Long-Term Care Residents
Rehab Patients
Through our patient-centered approach, we are able to improve the quality of life for residents and ensure they feel not only well-cared for, but also valued and significant.
By Park Manor Rehabilitation Center, Walla Walla, WA
We all know it’s true: There’s no place like home. That’s exactly what our 70-year-old female patient expressed upon  admission at Olympia Transitional Care and Rehabilitation.
admission at Olympia Transitional Care and Rehabilitation.
The patient experienced a cardiovascular accident at home resulting in a fall, with left distal femur shaft fracture. Upon admission, her level of function was as follows:
The patient lived at home with her spouse with multiple myeloma in a supportive, social community. She was independent with gait in her home and over short community distances; with swallow function, motor speech, functional cognition for her living environment; and with ADLs and IADLs, including cooking and cleaning.
This patient had one simple goal: “To get back to the way it was.” More specifically, she wanted to return home to her spouse and her cats, return to ambulation at household distances, and decrease the level of caregiver assistance for ADLs.
Treatment Approach
Taking an interdisciplinary approach, we developed a treatment plan combining physical, occupational and speech therapy. COTA and PTA created a “Passport to Home” document to visually track patient goals and progress:
Physical Therapy
Occupational Therapy
Speech Therapy
Additionally, we collaborated with nursing staff to ensure:
Conclusions
Using an interdisciplinary approach with complex patients is essential to realizing the highest level of performance success. The use of standardized testing allowed us to develop a personalized plan of treatment for this patient’s needs and improve the chances of a positive outcome.
Although this patient was quite discouraged at the onset of rehabilitation and did not have high expectations for success, we were able to encourage her along the way and improve her outlook. With a team approach, were developed a detailed treatment plan that ultimately allowed her to return home near her prior level of function.
By Scott Hollander, PT, PDT; Sarah Koning, MSOT, OTR/L; and Megan Bennett, MS, CCC-SLP, Olympia Transitional Care and Rehabilitation, Olympia, WA