Prior research has indicated that older adults treated with four weeks of reminiscence-structured activities to target specific personal memories showed fewer depressive symptoms, less hopelessness, improved life satisfaction and retrieval of more specific life events (Allen, 2009). Toward that end, we wanted to provide rehab patients and/or their caregivers with a value-added service — one that emphasizes a celebration of life and identifies the patient’s volition, rituals and habits through the use of a client-centered legacy-building intervention.
Prior research has indicated that older adults treated with four weeks of reminiscence-structured activities to target specific personal memories showed fewer depressive symptoms, less hopelessness, improved life satisfaction and retrieval of more specific life events (Allen, 2009). Toward that end, we wanted to provide rehab patients and/or their caregivers with a value-added service — one that emphasizes a celebration of life and identifies the patient’s volition, rituals and habits through the use of a client-centered legacy-building intervention.
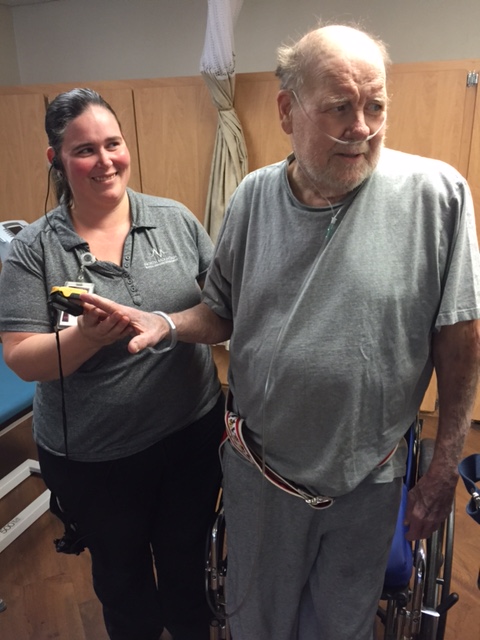
Through legacy-building activities, such as engaging with family members, creating slideshows, creating scrapbooks and creating videos, the patient and family improve existential awareness of their past, present and future. The goal is to improve activity tolerance, facilitate out-of-bed activities and address underlying deficits that influence ADL performance skills.
Partnerships and Collaborations
Our partnership with the Loma Linda University Occupational Therapy department, as well as other higher education institutions, allows us to recruit graduate-level fieldwork students to participate in our legacy-building project. By the end of week 12 (the end of fieldwork rotation), the FW II student presents a facility in-service regarding implementation and outcomes of the legacy-building program.
A Case Study in Legacy-Building
One patient, an 87-year-old woman, was admitted to Sea Cliff Health Care after a hospitalization secondary to generalized weakness, decreased functionality and decreased oral intake that revealed UTI, dementia, dehydration, coronary artery disease, anemia and urosepsis. The patient was evaluated by physical and occupational therapists for intervention once a day, five days per week, from March 24 to May 18, 2015.
Plan-of-care goals had to be modified throughout the process to address the patient’s increased aversive behaviors, outbursts and anxiety with therapy requests. We introduced behavioral modification techniques and legacy-building interventions, such as scrapbook making, a quote book and an interview for personal needs.
Thereafter, the patient met several functional goals and showed increases in other areas of ADL function, including BUE strength, seated balance, UB/LB dressing tasks and hygiene/grooming tasks. With the help of behavioral modification techniques and legacy-building interventions, the patient was able to demonstrate decreased aversive behaviors, confabulations, outbursts and anxiety and increased socialization (she sang more) without the use of psychotropic drugs.
Conclusion: a FW II Student’s View
Is the legacy-building project a valuable interpersonal teaching exercise? Why?
The experience during my level 2 fieldwork with the legacy-building project has allowed me to be a part of making a difference in the life of a patient that otherwise may have not had the means to advocate for their own care or means of participating in meaningful occupations at a vulnerable time in life.
What characteristics should future FW II students possess to be successful in this program?
It was important to be able to use therapeutic use-of-self in order to shape therapy sessions based on the patient’s needs and desires. Patience and empathy were also important characteristics for building rapport necessary to facilitate patient honesty, thoroughness and willingness to reveal personal anecdotes and experiences.
Did the program meet its objectives? The program reached its objectives to create mementos and informative aids for facilitating increased communication between patient and family/caregivers, while creating a product that is meaningful and can be used to maintain the patient’s legacy.
By Kristine Lewis MOT, OTR/L, Sea Cliff Health Care, Hungtington Beach, CA, In partnership with Loma Linda University OT Department