By Calli Carlson, OTR/L, DOR, North Mountain Medical & Rehab, Phoenix, AZ
“Oh it’s just basic range of motion. That patient doesn’t require therapy anymore.” I’m embarrassed to think of how often I have said these words, and I wonder how many therapists may relate to this same perception.
Previously in our facility, patients who were non-responsive or minimally responsive were transitioned from our skilled physical and occupational therapy to restorative nursing programs for passive range of motion, typically for three days a week. Over time, we began to notice that patients were demonstrating difficulty maintaining their current range of motion, while restorative nursing was likewise reporting increased tone and increased difficulty working with our more medically complex patients.
For patients with complex brain and spinal cord injuries, hypertonicity can worsen with time causing an invariable decline in range of motion as well as increased difficulty for restorative members performing their range of motion treatments and increased difficulty for certified nursing assistants performing basic tasks such as dressing and peri care. With this in mind, the dialogue began to shift from therapy could be involved in these patient cases to therapy should be involved in these patients cases to provide the best possible outcomes and improve quality of life.
Given the depth of therapists’ schooling on anatomy, neuroanatomy, kinesiology, positioning, and modalities, it seemed that therapists could provide enormous benefit simply by increasing their involvement and time with these clinically complex patients while also educating and instructing restorative nursing assistants, certified nursing assistants, and additional floor staff as needed.
A physical therapist at North Mountain Medical Center, Shannon Dougherty, took initiative and recently developed a program titled, “No pressure, no pain, no problem,” focused on improving the health and quality of life of long-term care residents in the facility. The 3-part program encompasses the following:
Part 1: No Pressure: Reducing likelihood of pressure injuries through bed positioning
Part 2: No Pain: Reducing pain through manual techniques, modalities, contracture management
Part 3: No Problem: Identifying ‘problem’ patients and completing CNA/RNA training for improved techniques, removing burden from RNA for especially complex patients that require additional assist.
The program is currently just beginning here at North Mountain, but we have already been surprised and encouraged by results we have seen thus far. One of our patients, in particular, presents with significant hypertonicity and accompanying flexion of upper and lower extremities at rest, placing this patient at high risk of developing contractures without appropriate intervention. Restorative nursing members have reported that this patient is typically averse to passive range of motion and that they have difficulty knowing how to properly complete this task. A formal therapy evaluation and subsequent treatment sessions identified that this particular patient responds well to simple verbal/tactile cueing, gentle massage of the hypertonic muscles, slow and prolonged stretch, as well as stretching muscles in isolation rather than combing several stretches at once (such as hip/knee extension). Therapists have begun educating restorative nursing members on these techniques as well as analyzing non-verbal pain responses such as diaphoresis, increased flexion posturing, facial grimacing, or increased heart rate in order to provide the best quality, patient-centered care.
The plan of care may differ for individual patients. For example, therapy might decrease restorative nursing visits to two times per week and see that patient once or twice per week to supplement their treatments, or therapy might work with that patient five days per week and discontinue restorative nursing at that time while they work to get a baseline and treatment ideas to share with the rest of the staff. Regardless of the method and scheduling, it is important that therapists see the value of their knowledge and skillset, restorative nursing members feel empowered and capable when working with these patients, and patients receive the best quality of care to improve their health and well-being while under our umbrella of care.





 Carly Peevers is an SLP out of Rosewood Rehabilitation in Reno, Nevada. Carly is passionate about giving great clinical care and has recently taken on an educational role within the Pennant, Idaho/Nevada, market.
Carly Peevers is an SLP out of Rosewood Rehabilitation in Reno, Nevada. Carly is passionate about giving great clinical care and has recently taken on an educational role within the Pennant, Idaho/Nevada, market.

 Kristin Ryther, the therapy program manager at Keller, has been a breath of fresh air in a very trying year at a facility that has been hit hard by COVID on multiple occasions. We asked her to share a bit of her best practices and were blown away by what is developing there.
Kristin Ryther, the therapy program manager at Keller, has been a breath of fresh air in a very trying year at a facility that has been hit hard by COVID on multiple occasions. We asked her to share a bit of her best practices and were blown away by what is developing there. gratitude. Kristin has become a champion of championing others. She works to identify strengths in each of her team members and then assigns responsibilities appropriately. Each member has a strength; slow down and find it! It may be that they have special attention to individual treatments; they may be strong at scheduling, growing programs, or even leading the infection control of the gym. List them out and recognize them.
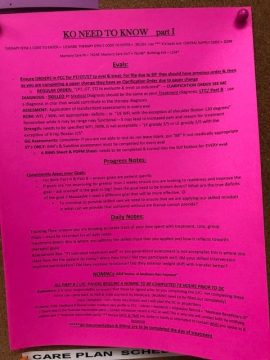
gratitude. Kristin has become a champion of championing others. She works to identify strengths in each of her team members and then assigns responsibilities appropriately. Each member has a strength; slow down and find it! It may be that they have special attention to individual treatments; they may be strong at scheduling, growing programs, or even leading the infection control of the gym. List them out and recognize them.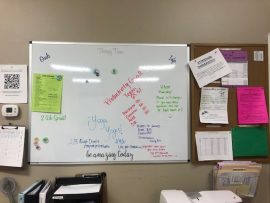 Set clear goals and expectations. Kristin sets goals for “2 week sprints.” Some programs are short projects. She assigns a leader and assists with facilitation but allows for teamwork so they meet their goals. She posts the sprints on the communication board, writes about it, takes pictures and then celebrates it. Short-term goals like this make it manageable, and then the challenge is less likely to be pushed off down the road.
Set clear goals and expectations. Kristin sets goals for “2 week sprints.” Some programs are short projects. She assigns a leader and assists with facilitation but allows for teamwork so they meet their goals. She posts the sprints on the communication board, writes about it, takes pictures and then celebrates it. Short-term goals like this make it manageable, and then the challenge is less likely to be pushed off down the road.