When it comes to our long-term care patients, many of our standard tests simply do not serve them well in regards to monitoring subtle changes over time. Standard tests such as the BERG, DGI and Tinneti are not good for patients who are wheelchair-bound. Additionally, using these tests as short-term goals can create challenges, as the patient’s overall scores will remain relatively unchanged for several weeks in most cases.
In contrast, the Physical Mobility Scale (PMS) can be used to help determine improvements and declines in function, as it measures a wider range of functional skills. The PMS measures nine basic movements using an ordinal scale of 0 to 5 for a total of 0 to 45 possible points.
Article Review
Pike and Landers (2010) studied 70 LTC residents to determine the minimal detectable change (MDC) for the PMS. The same therapist was used for all tests. Residents were tested three months apart, and a 7-point Likert Scale (very much improved to very much worsened) was used to determine how much change indicated 95 percent confidence level (MDC95).
Results
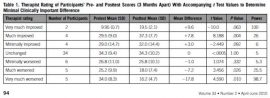
Table 1 shows the ratings of the pre- and post-tests (three months apart).
Data
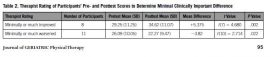
It was found that a 5-point increase and a 4-point decrease showed a minimal clinically important difference at the 95 percent confidence level (MDC95). The scores that reflected no change were removed, and all improved scores and worsened scores were combined into two separate categories as seen in table 2.
Conclusion
The Physical Mobility Scale is reliable, easy to use and understand, covers all the basic skills of our patients and has high validity. This standardized test will show steady progression over time and can be used to determine increases and decreases in our long-term and short-term residents.
By Scott Langdale, PT/DPT, DOR, Beacon Hill Rehabilitation, Longview, WA
