By Lori O’Hara, MA, CCC-SLP, PDPM Resource
One of the miraculous things about PDPM is that we are incentivized to go learn things! And … we have the patient with us, 24/7, sometimes for weeks! There is no other provider — not the acute, not home health, not outpatient, not anyone who gets to have their arms around the patients as closely as we do and who are also told to go learn absolutely as much as we can.
Just us, baby!
So this presents an incredible opportunity to be the best assessors, the best investigators and the best, most impactful providers a patient will come into contact with.
This means that we if work superficially — if we’re content with just the diagnoses on the transfer list and just the treatments that come to us — that we’ll miss out on the potential for incredible impact to a patient, which, super conveniently, is pretty reimbursable when we do it.
So part of being a PDPM Ninja is knowing where the arrows are pointing. What conditions tend to come in clusters? What treatments should we be advising the MD that we can do? What low-impact, non-invasive interventions could have a big payoff for this patient if we just think about doing them?
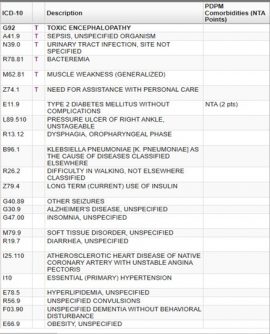
So here’s an exercise for you. Look at the diagnosis list below. And before you scroll down, think through all the “maybes.” What might related conditions be? What treatments should be considered? What condition might mask another where you should take a close second look?
So what did you find?
Here’s what I found:
-
-
-
- Sepsis and Bacteremia = Need records to confirm or r/o septicemia
- Diabetes and insulin = Check for diabetic retinopathy and proactive management of insulin regimen in case order changes are needed
- Diarrhea = Investigate source (radiation, infection, c-diff?) to confirm or r/o inflammatory bowel disease
- Convulsions and seizures = Investigate control status (25% of seizure disorders are poorly controlled/intractable)
- Klebsiella PNA and sepsis = Query for labs for drug resistance status
- Alzheimer’s disease and encephalopathy = Cognitive impairment
- Obesity = Score BMI, assess if patient’s weight warrants morbid obesity diagnosis
- PNA = Assess for need for RT interventions
- UTI = Assess voiding and s/s of retention for straight cath medical management
- Multiple malnutrition markers present (infections, dementia, diarrhea, dysphagia)
- Dysphagia = Should trigger on Section K, which should then correlate to altered texture diet trigger for altered texture diet
-
-
Did you spot any others? You can also do this exercise with medical documentation from the upstream provider. And the more clinical brains, the better! Each clinician carries their own training and experience into the room, so one brain might pick up on something another brain might not spot. And when you find four or five “maybes,” you know that not every one of them will result in a new condition to code and care for. But you’ll probably find a thing or two, and maybe find something else — completely unrelated to payment — that will have a big impact on your patients’ health and recovery.
Like I said — miraculous!
