Submitted by Tamala Sammons, M.A., CCC-SLP, Therapy Resource
 The Mission:
The Mission:
Improve Sepsis identification early to improve patient outcomes.
The Why:
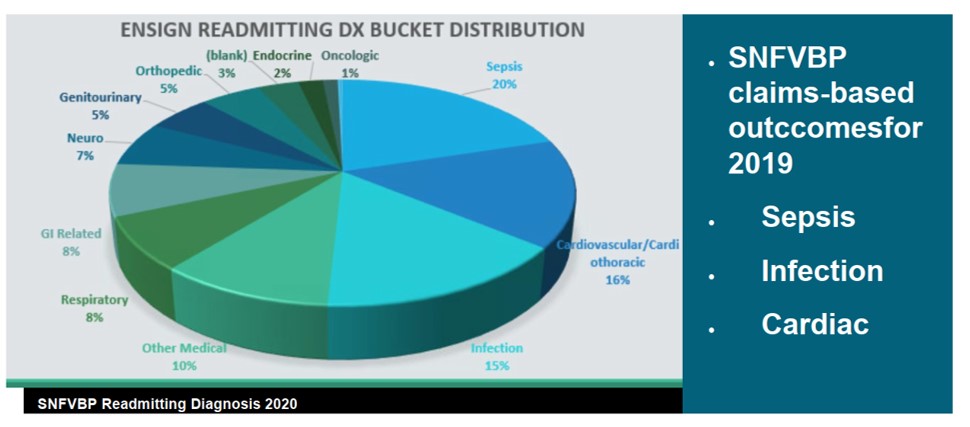
Sepsis was 20% of our Medicare Readmissions as an Organization in Calendar Year 2019.
With every hour that treatment is delayed for sepsis, the mortality rate increases by 8%. Understanding and educating our facilities on SIRS and a focused vital-sign campaign with an SBAR-specific focus will improve our care delivery and reduce readmissions, improve our patient satisfaction, and help with our change in condition process.
COVID-19 and Sepsis: A Physician’s Lens
While there is still a lot to uncover about the pathology and presentation of COVID-19, we have learned a great deal about this virus and its potential impact in our post-acute care facilities. During our experience at one of the early COVID-19 outbreak facilities, it was discovered that an early presentation of many COVID-19 patients was the presence of a fever. Unfortunately, these fevers were managed with the typical order for acetaminophen and cooling measures, effectively masking the fever and avoiding any further escalation of care until the patient reached a point of medical instability. Sepsis POSTette
Sepsis POSTette
As with any patient in a post-acute care facility presenting with fever, even before COVID-19, timing is absolutely critical. Other changes of condition such as chest pain or possible stroke have led to long-standing, conditioned responses to immediately send patients out via 911. Fever is often the hallmark sign signaling the beginning of a patient experiencing sepsis — a diagnosis that carries a much higher chance of mortality, especially in the post-acute care population, but up until now has not received the attention it deserves. Oftentimes a febrile episode is masked or ignored, leading to a cascade of events leading to further demise, accelerated by a virus that now has the potential to spread like wildfire.
We are now at a point where identification of fevers (and other changes of condition) should signal a “code” event, essentially alerting the clinical team to provide immediate identification, isolation, and intervention. With every hour that a fever is ignored, the mortality rate for a potential sepsis patient increases by 8%. This simple, yet widely underappreciated clinical practice can prove to be a pivotal step in reducing the mortality in not just our COVID-19 patients, but in any patient who is on the path of developing sepsis. — Dr. Pouya Afshar
For more information, click here for our Sepsis POSTette




 By Jack Rolfe, PT, MNA, CHC, RAC-CT, Senior Compliance Partner for Utah
By Jack Rolfe, PT, MNA, CHC, RAC-CT, Senior Compliance Partner for Utah
 By Shelby Donahoo, M.S., OTR/L, Therapy Resource – Bandera
By Shelby Donahoo, M.S., OTR/L, Therapy Resource – Bandera