Here are some in room therapy treatment suggestions from our Keystone Resources:
● “Boxing” while supine in bed to work on trunk rotation, rolling side to side for bed mobility, UE strength and activity tolerance; add weights if appropriate
● “I Spy” game for word finding/verbal reasoning goals
● Bird identification out the window. Laminate photos of birds/scavenger hunt looking out window
● Cleaning the bathroom mirror
● Decorating or making a calendar for orientation
● Decorating the room
● Drawing, window painting/drawing
● Fall recovery
● Folding laundry
● Game cards and play this while standing to add in cognition component
● Have a therapist in the hallway and have some residents in the doorway and do some deep breathing and gentle exercise! Maybe have some questions to help facilitate conversation.
● Have some pictures ready for them; have them pick a picture from the pile and have them describe it to you!
● Have them tell us a hobby and modify it for them! We are super creative!
● If they have flowers in their room, trim them and replace the water. This can be done sitting or standing. If they are higher level, have them sweep up the fallen leaves and petals.
● Instructing patients in correct hand-washing techniques
● Introduce HRV training to help relieve anxiety during this time
● Item retrieval/transport
● Making the bed
● Making a collage with family pictures
● Making a cool Easter egg balloon with yarn to hang in their room
● Making cards for their loved ones
● Organize closet by colors/season of clothes
● Painting on paper
● Place patient’s clothes around the room at various levels, have them walk around and gather items, make decisions on whether to use reacher or not, manage reacher and RW, energy conservation education regarding rest breaks, etc.
● Plant something in a flower pot to put in the window sill for them to watch grow
● Postural exercises, high/low reaching

● Put laundry on hangers and hang in closet (gross/fine motor and reaching)
● Scavenger hunt in room (list of objects to find)
● Small space functional mobility
● Talk about their life while they are rocking their wheelchair back and forth 🙂. They need to feel calm.
● Teaching them how to use the phone, FaceTime, and trying with a loved one … which brings happy tears, messenger on FB has a video chat as well, so setting them up to keep in touch with loved ones. Also, setting up a free music app on their phone, or a simple game like solitaire.
● Wall pushups working on posture
● Washing windows
● Wheelchair mobility “obstacle course” having to navigate around actual items and furniture in room
● Wheelchair pushups (5xSTS test)
Sequencing for sit to stand (brakes on, scoot up to edge of seat, back, hands in arm rest, fwd trunk nose over toes, 1, 2, 3, push up thru arms and LEs!). Get picky; perfect practice is the only way to instill good habits and break bad habits.
Sequencing for stand pivot transfers with assistive device
Standing balance (Romberg test), standing scalp retracts for stability, steps fwd, lateral, retro
Berg/Tinetti/TUG tests can be done in patient’s room and some aspects of them if anything can be worked on like 360-degree turns in place or picking object up from floor, etc.
● Writing letters/cards/postcards to loved ones
● Use AAC device to give instructions on how to set up/decorate the room; use patients’ phones or tablets for higher-level problem solving (e.g., sequencing steps to write a message on a niece’s Facebook timeline); use their phones/tablets to teach them to set up external memory aids (ex- add doctors’ numbers to contact list, set daily alarms for times they need to take meds); help them set up a grocery delivery acct for when they discharge home; use dysarthria (or aphasia or voice!) techniques during functional phone calls (talk to family, pay bills via phone, etc.); use objects in room for receptive language tasks (“Point to the razor THEN pick up the comb”).



 We invite anyone who is able and interested to join us with HeartMath at 8:30 a.m. Pacific daily during this time. Totally optional! You can join for one minute or join for longer. We would like to use the “Global Coherence App” that is available for free to download if you are able! Here are the instructions:
We invite anyone who is able and interested to join us with HeartMath at 8:30 a.m. Pacific daily during this time. Totally optional! You can join for one minute or join for longer. We would like to use the “Global Coherence App” that is available for free to download if you are able! Here are the instructions:

 Discovering running at a much later stage in life has been the greatest gift life has given me. It came at a perfect time when I needed a lift, to be reminded of my life’s purpose and overcome my self-imposed limitations. Running has given me everything … my renewed self-love, my self-confidence, my fearlessness, my grateful attitude and my purpose. It has inspired my new direction and outlook. It has taught me to push forward when things get difficult. In return, I am giving it my heart.
Discovering running at a much later stage in life has been the greatest gift life has given me. It came at a perfect time when I needed a lift, to be reminded of my life’s purpose and overcome my self-imposed limitations. Running has given me everything … my renewed self-love, my self-confidence, my fearlessness, my grateful attitude and my purpose. It has inspired my new direction and outlook. It has taught me to push forward when things get difficult. In return, I am giving it my heart. In March 2017, I ran my first individual race, which was a half marathon with my sister. We decided to follow the 2:30 pacer. I wasn’t serious about it at first, conversing with her while running, answering texts during the race until around mile 8-9 when I saw how serious and competitive other runners were and thought to myself that maybe I should take it more seriously, too. I started giving it my best and got ahead of the 2:15 pacer to the finish. This race gave me a glimpse of the possibilities, although a full marathon was still out of the picture at that time.
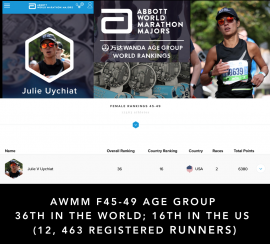
In March 2017, I ran my first individual race, which was a half marathon with my sister. We decided to follow the 2:30 pacer. I wasn’t serious about it at first, conversing with her while running, answering texts during the race until around mile 8-9 when I saw how serious and competitive other runners were and thought to myself that maybe I should take it more seriously, too. I started giving it my best and got ahead of the 2:15 pacer to the finish. This race gave me a glimpse of the possibilities, although a full marathon was still out of the picture at that time. currently chasing the 6 Major Marathons in the world and since 2018 have completed four of six (Berlin, Chicago, Boston and New York). From these races, I have earned a respectable world ranking and received an invite to run the Wanda Age Group World Championships inaugural race in London this April. This is where I will be competing against 84 other top world runners in my age group.
currently chasing the 6 Major Marathons in the world and since 2018 have completed four of six (Berlin, Chicago, Boston and New York). From these races, I have earned a respectable world ranking and received an invite to run the Wanda Age Group World Championships inaugural race in London this April. This is where I will be competing against 84 other top world runners in my age group.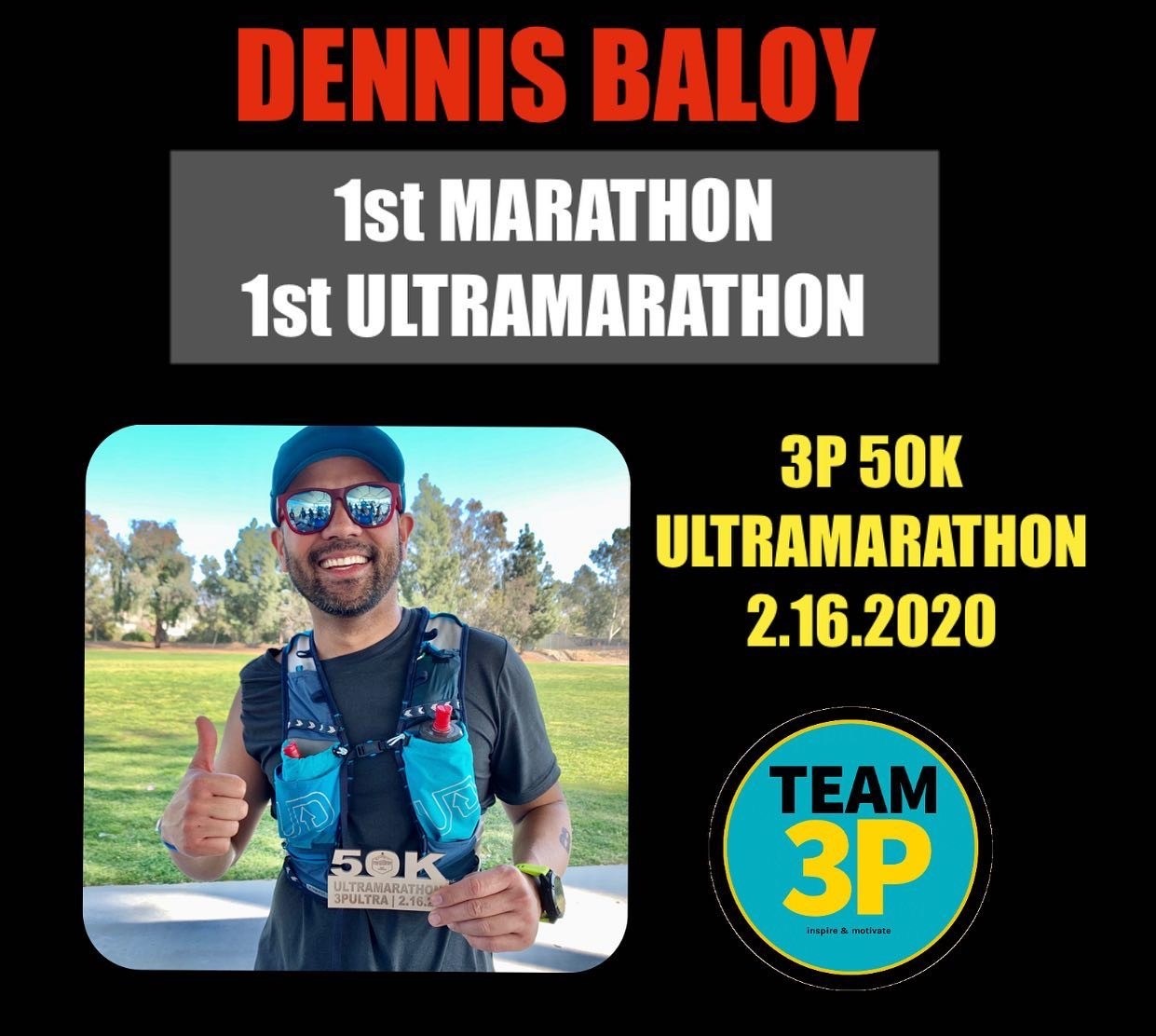

 When looking at what programs haven’t been tapped into, my ED and I decided to focus on outpatient and what we could do differently to get our program back up and running again. Outpatient at Vista Knoll Specialized Care has always been something that was never really focused on and was getting by with minimal referrals over the past few years. To start, we looked at our outpatient census and how we could gain more referrals. With that, we decided to make our rehab tech, Diana, the outpatient champion.
When looking at what programs haven’t been tapped into, my ED and I decided to focus on outpatient and what we could do differently to get our program back up and running again. Outpatient at Vista Knoll Specialized Care has always been something that was never really focused on and was getting by with minimal referrals over the past few years. To start, we looked at our outpatient census and how we could gain more referrals. With that, we decided to make our rehab tech, Diana, the outpatient champion.

 The sound of light drumming and laughter filters down the hallway as the residents and patients start to assemble for drum circle. “I like chocolate cake, that’s the beat we’re going to play,” instructs Amy Pot, Director of Rehab, and Lulu Matos, Director of Activities, to a group of residents and patients at Palomar Vista Healthcare Center. They are drumming along on Turbano drums to I Love Rock and Roll by Joan Jett.
The sound of light drumming and laughter filters down the hallway as the residents and patients start to assemble for drum circle. “I like chocolate cake, that’s the beat we’re going to play,” instructs Amy Pot, Director of Rehab, and Lulu Matos, Director of Activities, to a group of residents and patients at Palomar Vista Healthcare Center. They are drumming along on Turbano drums to I Love Rock and Roll by Joan Jett.