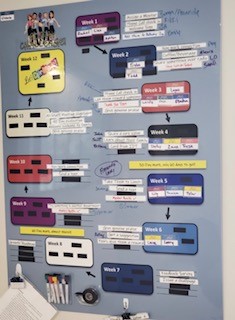
A Capstone Project by Melissa Alexander, M.A. CCC-SLP, Opus and Millenium Post Acute Care, West Columbia, SC
At Millennium Post-Acute care we wanted to make sure the importance of oral infection control was integrated effectively at our facility. Did you know that tooth brushing prevents more than just cavities and bad breath? Poor oral hygiene has been related to a number of medical conditions including:
• Diabetes mellitus
• Cardiovascular disease
• Strokes
• Atherosclerosis
• Myocardial infarction
• Cancers, including:
• Kidney (risk increased by 49% in men)
• Pancreatic (risk increased by 54% in men)
• Blood (risk increased by 30% in men)
• Pregnancy complications such as low birth weight and prematurity9
• Pneumonia
Oral Health Status can be determined by examining the teeth, tongue, and mouth. The Oral Health Assessment Tool (OHAT) is a recognized, proven screening tool for just that purpose. By implementing a strong oral infection control program we have also been able to have more patients on Free Water Protocols and are helping ensuring adequate hydration. By working together, we are putting attention on quality oral care to prevent infections that lead to adverse medical conditions. Education was key including information on the effects of poor oral hygiene, the pros and cons of toothettes and the basics of good oral care.
Source: American Academy of Periodontology. (n.d.). Gum Disease Information. Retrieved July 1, 2018, from https://www.perio.org/consumer/gum[1]disease.htm
Additional Resources: POSTettes Reducing Risk of Dehydration / Free Water Protocol and Oral Health Assessment Tool for Non-Dental Professionals