![]() By April Trammell, SLP, DOR, Beacon Harbor Health & Rehabilitation, Rowlett, TX
By April Trammell, SLP, DOR, Beacon Harbor Health & Rehabilitation, Rowlett, TX
Jimmy arrived at Beacon Harbor on April 13, 2020. He was in a very devastated state following a spinal fusion, which was compromised, leaving him with hemiparesis from the chest down. Because he was unable to feel his legs and feet, he was having frequent falls, required a hospital bed with assist rails in order to maneuver in and out of bed, and was wheelchair-bound. “I was brought to Beacon Harbor for my last days on earth to be comfortable and to give my wife Dianne a respite.”
Plans for Jimmy were to transition here to Beacon Harbor long-term care. But Jimmy had other plans in mind. He was successfully determined to wean off of all pain medication. “Then I started doing therapy — that wore me out — but I had it in my head that I wanted to recover.” Jimmy and his team of therapists were determined to help him gain his independence. “Day after day, week after week, I started improving not just a little bit — a lot! No explanation ‘why’ except my therapy and my willingness to do what is asked of me. They have challenged me on so many things, and they are holding me up, allowing me to improve.” He progressed to being able to transfer independently in and out of bed, and to be able to complete basic self-care such as dressing, bathing and toileting independently. “I feel like I am being rebuilt. There’s something about this place that draws it out of you.”
Jimmy and his therapists continued to focus on neuro re-education, and he slowly began to regain full sensation in his body. “I am able to feel hot water and take a hot shower for the first time in over 35 years!” He did not give up; Jimmy continued to thrive in therapy and began walking with a walker for the first time in 10 years. “I started taking control of my life slow, but every day it was a very hard road to walk down — for myself, for my wife and family. I would say Beacon Harbor is just one of the best rehab centers that I’ve ever been in in this nation, and I have been in quite a few from state to state over the years. The bottom line, Beacon Harbor: You have an amazing PT, OT, ST and Nursing staff. I’m getting ready for my second phase of taking my life back. I’m going to move into assisted living, and from there, back home. Thank you for a second chance at life.”

 This is our first group treatment since October, which is when we went into full lock-down, outbreak mode. It was organized by two of the most compassionate therapists I know, Emily White, PTA, and Wendy Garrison, OTA. The residents had a blast!
This is our first group treatment since October, which is when we went into full lock-down, outbreak mode. It was organized by two of the most compassionate therapists I know, Emily White, PTA, and Wendy Garrison, OTA. The residents had a blast! This is Ron; he was in a catastrophic car accident in 2019, which brought him to us. He received prosthetic training and was set to go home in early November, when he tested positive for COVID. Plans to DC home were postponed, but he made it, and has made it back home to Nebraska.
This is Ron; he was in a catastrophic car accident in 2019, which brought him to us. He received prosthetic training and was set to go home in early November, when he tested positive for COVID. Plans to DC home were postponed, but he made it, and has made it back home to Nebraska. This is Jessica, the Clinical lead and head cheerleader for team Ron. We all cried like babies when he finally went home.
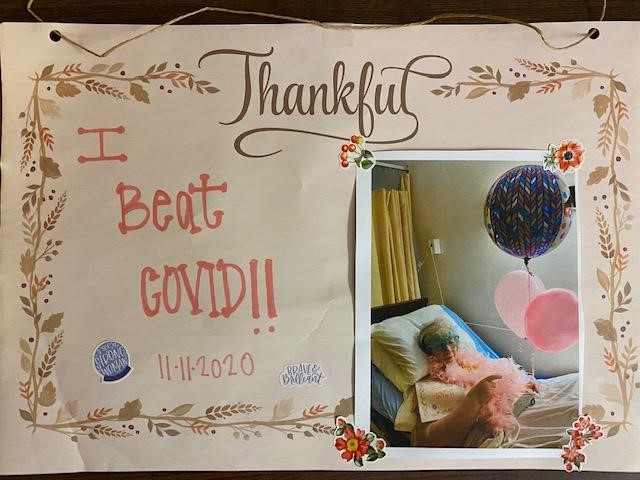
This is Jessica, the Clinical lead and head cheerleader for team Ron. We all cried like babies when he finally went home. As a compromised patient, Glenna should not have survived, according to all our knowledge of the virus, but she did. What a happy day it was to move her off of the COVID wing back to her own room.
As a compromised patient, Glenna should not have survived, according to all our knowledge of the virus, but she did. What a happy day it was to move her off of the COVID wing back to her own room. This was our very first survivor. She didn’t even know she was sick and was happily confused about all the fuss we were making over her. We are all truly thankful for the opportunity to celebrate with her. (photo of thankful I beat COVID)
This was our very first survivor. She didn’t even know she was sick and was happily confused about all the fuss we were making over her. We are all truly thankful for the opportunity to celebrate with her. (photo of thankful I beat COVID)
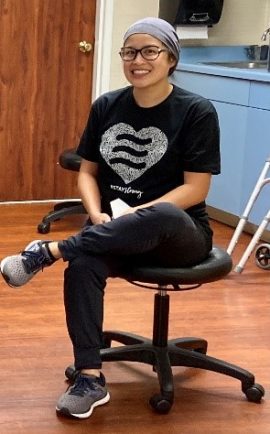 Denise Del Cano, COTA, ADOR, has dedicated her career in The Hills Post Acute. An alumnus of Santa Ana College, she earned her associate’s degree in Occupational Therapy Assistant 12 years ago and has been with the facility since then. She was promoted to Assistant Director of Rehab last year and completed the DORITO program this year. Denise did her internship here at The Hills. She was supervised by Vonda Gaier, COTA, who then became her colleague. She is a Filipino American born in Los Angeles, California, the eldest of five and a loving mother to her 16-year-old daughter, Elizabeth. Interestingly, Denise was introduced to the field of therapy when her daughter received therapy for several years. Denise saw the importance and relevance of Occupational Therapy and has been an advocate ever since.
Denise Del Cano, COTA, ADOR, has dedicated her career in The Hills Post Acute. An alumnus of Santa Ana College, she earned her associate’s degree in Occupational Therapy Assistant 12 years ago and has been with the facility since then. She was promoted to Assistant Director of Rehab last year and completed the DORITO program this year. Denise did her internship here at The Hills. She was supervised by Vonda Gaier, COTA, who then became her colleague. She is a Filipino American born in Los Angeles, California, the eldest of five and a loving mother to her 16-year-old daughter, Elizabeth. Interestingly, Denise was introduced to the field of therapy when her daughter received therapy for several years. Denise saw the importance and relevance of Occupational Therapy and has been an advocate ever since. As we persevere through the pandemic, I am often reminded how fortunate I am to have such wonderful teammates. I continue to be the proudest team leader.
As we persevere through the pandemic, I am often reminded how fortunate I am to have such wonderful teammates. I continue to be the proudest team leader.



 By Milena Milenkovic, OT/DOR, Park View Post Acute, Santa Rosa, CA
By Milena Milenkovic, OT/DOR, Park View Post Acute, Santa Rosa, CA
 On March 13, 2020, President Trump declared a national emergency, citing an outbreak of COVID-19. On that same day, CMS strictly restricted in-person visitation to only compassionate care situations in skilled nursing homes in order to prevent the introduction of COVID-19 to our most vulnerable population: the elderly with pre-existing medical conditions.
On March 13, 2020, President Trump declared a national emergency, citing an outbreak of COVID-19. On that same day, CMS strictly restricted in-person visitation to only compassionate care situations in skilled nursing homes in order to prevent the introduction of COVID-19 to our most vulnerable population: the elderly with pre-existing medical conditions.
 Here at Golden Acres in Dallas, Texas, we love our long-term care residents. They are the heart and soul of our facility, and we wouldn’t have it any other way. One of our residents passed away recently, and it never gets easier. The family reached out to myself, the DOR, and the social worker in hopes of getting a copy of her grandmother’s life storyboard that was created during therapy with one of our amazing speech therapists. Her granddaughter wanted to utilize this resident’s life storyboard to aid in writing her obituary. To think that the Abilities Care Approach Program could, in such a trying and upsetting time, bring joy and meaning to a grieving family is truly amazing.
Here at Golden Acres in Dallas, Texas, we love our long-term care residents. They are the heart and soul of our facility, and we wouldn’t have it any other way. One of our residents passed away recently, and it never gets easier. The family reached out to myself, the DOR, and the social worker in hopes of getting a copy of her grandmother’s life storyboard that was created during therapy with one of our amazing speech therapists. Her granddaughter wanted to utilize this resident’s life storyboard to aid in writing her obituary. To think that the Abilities Care Approach Program could, in such a trying and upsetting time, bring joy and meaning to a grieving family is truly amazing.