By Brian del Poso, OTR/L, CHC, RAC-CT and Tamala Sammons, MA, CCC-SLP, Therapy Resources
Sensory Integration (SI) Therapy was originally invented by OT, Jean Ayres, in the 1970s to help children with sensory processing problems. Although less prevalent, SI techniques and theory used to modulate the sensory and proprioceptive systems can also be used with the adult population.
We’ve had a few questions recently around the appropriate use of the 97533 Sensory Integration CPT code. In general, this is an allowable code and covered by our MACs. However, since we know SI is predominantly used with the pediatric population, if utilizing this code as part of therapy intervention with the adult population, it is important that we use evidence-based practice, research, and have clear supportive documentation to demonstrate that sensory processing/modulation is a cause of functional deficits and that the interventions being billed truly fall within SI intervention strategies.
Here is the Sensory Integration 97533 code descriptor:
This activity focuses on sensory integrative techniques to enhance sensory processing and to promote adaptive responses to environmental demands, with direct one-on-one contact by the qualified professional, each 15 minutes.
From AOTA:
“Occupational performance difficulties due to sensory modulation challenges or poor integration of sensation can result from difficulties in how the nervous system receives, organizes, and uses sensory information from the body and the physical environment for self-regulation, motor planning, and skill development. These problems impact self-concept, emotional regulation, attention, problem solving, behavior control, skill performance, and the capacity to develop and maintain interpersonal relationships. In adults, they may negatively impact the ability to parent, work, or engage in home management, social, and leisure activities.”
From the AOTA article: Sensory Integration Use with Elders with Advanced Dementia
“Research of current approaches in treating older adults with dementia to decrease negative symptoms and increase quality of life, revealed the trend of using a multi-sensory protocol designed for this population (Chitsey, Haight, & Jones, 2002; Knight, Adkison, & Kovach, 2010; Kverno et al., 2009; Lape, 2009; Letts et al., 2011; Padilla, 2011). Kverno et al. (2009) noted in their literature review of non-pharmacological treatment of individuals with dementia that “individuals with advanced levels of dementia benefited to a greater extent from nonverbal patterned multisensory stimulation” (p. 840). Multisensory stimulation incorporates the use of tactile, visual, auditory, olfactory, and gustatory sensory pathways, along with movement, to help the individual interpret his or her environment (Lape, 2009).”
The occupational therapy evaluation and treatment plan is designed to “structure, modify, or adapt the environment and to enhance and support performance” (American Occupational Therapy Association, 2015, p. 6913410050p1), in order to re-engage patients.
Adding sensory integration as a treatment approach starts with assessing any comfort or discomfort when a patient is participating in: ADLs (grooming, dressing, bathing, etc.); Meals; Upper extremity movement; Functional transfers; Seating and positioning.
Goals can be developed around any identified areas of discomfort by creating situations to increase episodes of comfort with those tasks.
What do the MACs say? Here is the language from the Novitas as an example:
Sensory Integration 97533
This activity focuses on sensory integrative techniques to enhance sensory processing and to promote adaptive responses to environmental demands, with direct one-on-one contact by the qualified professional, each 15 minutes.
The patient must have the capacity to learn from instructions. Utilization of sensory integrative techniques should be infrequent for Medicare patients.
For more resources, documents, and tools to help provide information to you and your staff, please see the Sensory Integration section under Therapy > Clinical Programming on the Portal.


 Why is respiratory function so important for SLP involvement?
Why is respiratory function so important for SLP involvement?


 Carly Peevers is an SLP out of Rosewood Rehabilitation in Reno, Nevada. Carly is passionate about giving great clinical care and has recently taken on an educational role within the Pennant, Idaho/Nevada, market.
Carly Peevers is an SLP out of Rosewood Rehabilitation in Reno, Nevada. Carly is passionate about giving great clinical care and has recently taken on an educational role within the Pennant, Idaho/Nevada, market.
 When Sara Mohr, CFY at Sabino Canyon in Tucson, Arizona, was a SLP graduate student at the University of Arizona, the reality for those on modified diets became clear. Often a diagnosis of dysphagia brings confusion and worry. Getting modified diets right seems obvious, but actually can be quite hard. Options seemed few: mashed potatoes, blended meat and yogurt. She found few resources out there for patients in terms of appealing and tasty recipes with easy instructions for cooking and modifying.
When Sara Mohr, CFY at Sabino Canyon in Tucson, Arizona, was a SLP graduate student at the University of Arizona, the reality for those on modified diets became clear. Often a diagnosis of dysphagia brings confusion and worry. Getting modified diets right seems obvious, but actually can be quite hard. Options seemed few: mashed potatoes, blended meat and yogurt. She found few resources out there for patients in terms of appealing and tasty recipes with easy instructions for cooking and modifying.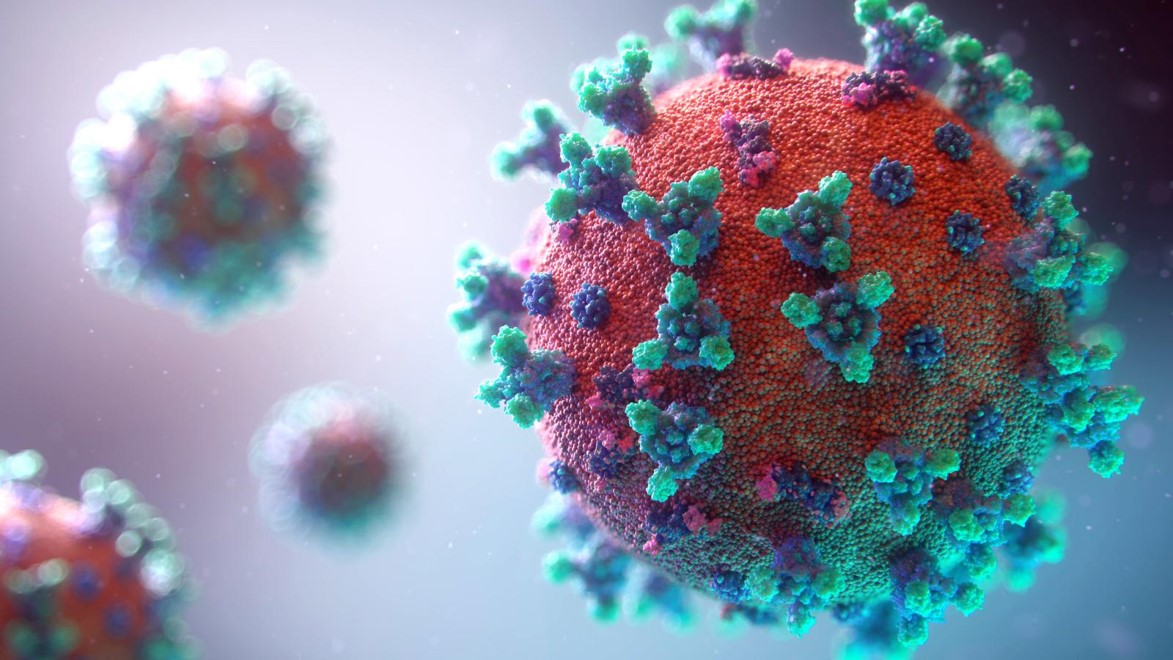
 COVID-19 is a respiratory viral disease with multi-organ involvement resulting in potentially temporary and episodic health challenges such as impaired lung function, physical deconditioning, cognitive impairments, impaired swallow and communication, and mental health disorders.
COVID-19 is a respiratory viral disease with multi-organ involvement resulting in potentially temporary and episodic health challenges such as impaired lung function, physical deconditioning, cognitive impairments, impaired swallow and communication, and mental health disorders.
