By Gary McGiven, Milestone Therapy Resource, Utah
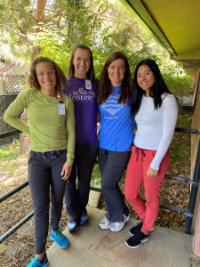
Nicole Newberry was the DOR at Draper Rehab for the last 15 months. Early on in her experience as a DOR, she saw the value of having an ADOR and growing leaders. As a result of this realization, she identified a member of her team that she wanted to help grow as a leader. Jamie Sack, SLP, was the natural choice, as Jamie has been completely bought into the growth of the therapy program at Draper.

Over the last year, Jamie has participated in the DORiTO program, learned the daily technical, weekly skilled review, triple check process, and spent about eight weeks filling in for Nicole while she was on maternity leave. While Nicole was on leave, we learned that she would be moving her family to St. Louis so her husband could complete a medical school fellowship in pediatric ENT. While we were saddened by the news that Nicole would be leaving us, we immediately were excited by the thought that Jamie would be able to seamlessly take over the role of DOR. With some further education on the DOR role provided to Jamie and Jamie explaining some of her expectations, we were able to solidify Jamie as the DOR for Draper Rehab.
Jamie was officially named the DOR a few weeks ago as sort of a Co-DOR. The week of June 21 was her first full week as the DOR of Draper Rehab. She has hit the ground running, and the transition to date has truly been seamless.
Going through this process made me realize the benefits of growing leaders and preparing/training your potential replacement. Most obviously, this makes the process seamless, as the future leader learns the systems needed to be an effective DOR and is given an opportunity to develop relationships with members of the Therapy and interdisciplinary teams.
In addition to the obvious, this allowed Jamie to see some of the challenges of the DOR role. As Jamie saw these challenges and more of the ins and outs of being a DOR, she has been able to set boundaries for herself to ensure she enjoys a greater work/life balance. We are so thankful for Nicole and Jamie and look forward to the great things Jamie will do as she continues to learn the DOR role.